When the GOP announced the first part of their new healthcare plan last week, one of the first things that many people noticed was the slashing of Medicaid. For the opioid and addiction epidemic, this could spell disaster. One estimate puts the number of people covered by Obamacare’s Medicaid expansion with mental health or substance abuse issues at over one million.
With 91 people dying everyday from an opioid overdose according to CDC data, coverage of addiction services is needed now more than ever. IMS Institute For Healthcare Informatics data reports that 1 out of every 4 prescriptions for Suboxone are paid for by Medicaid. But because insurance varies so much from state to state, it’s hard to predict across the board how the decimation of the Medicaid program will affect addiction treatment.
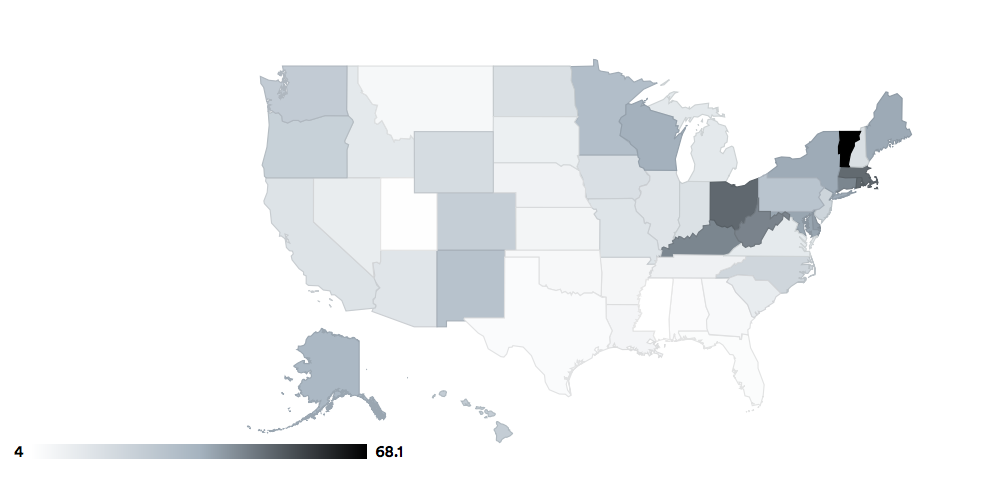
STAT News analyzed data to estimate the percentage of addiction treatment medication that is paid for by Medicaid in each state–to provide a picture of which states have the most to lose if Medicaid is overhauled. It ranged from just 4% in states like Utah and Mississippi to more than 68% in Vermont. California is 16%, Texas is 5.7%, Ohio is 49.5%, and Kentucky is 44.2%.

Map courtesy of Natalia Bronshtein/STAT
These disparities among states do not just occur when it comes to addiction treatment medications—they also exist in regard to treatment itself. As The Fix reported last year, despite the Affordable Care Act requiring all states to cover addiction treatment services, some were less than willing to pay for inpatient treatment.
States with expanded Medicaid were able to choose which levels of treatment they would cover: outpatient, intensive outpatient, inpatient, or intensive inpatient for detox. Twenty-six states covered at least one service on each level but nine states didn’t provide even a single option for care at two of the levels.
But the expansion of the Medicaid program allowed greater numbers of people to access treatment and, like the addiction treatment medications, the numbers varied from state to state. For some states, like Massachusetts, repealing Medicaid would be devastating for folks in the throes of addiction because treatment for so many residents of the state is covered by Medicaid expansion (and almost half of addiction treatment medication prescriptions—49.3%—were covered under Medicaid).
According to the IMS data, 24% of total Suboxone prescriptions nationally are covered by Medicaid. More than 40% of these prescriptions are covered by Medicaid programs in eight states, and 12 states have less than 10% covered.
