I’ve grown out of my shell, but not without a struggle. Not long ago, I was ashamed to share my story. Stigma is a strong barrier. But with loving support, I’ve been pushed into spaces where sharing my lived experiences can be empowering.
I used heroin for over a decade. For nine years, I tried to navigate my way toward long-term recovery. I finally made it, but not without trauma, lost relationships, life on the streets, and more than a little time behind bars. To quote a favorite TV character, “I took the long way ‘round.”
If I’d known then what I know now, I might have avoided all that. If my friends had known, they might still be alive.
1. Multiple Paths to Recovery
This is something many of us only learned in recent years, as peer support groups and treatment programs like SMART Recovery, LifeRing, SOS Sobriety, Women (and Men) for Sobriety, Moderation Management and HAMSgrow (see my reality-based recovery guide for more).
For decades, Twelve-Step recovery was the standard model. This isn’t an attack on that. It’s an acknowledgement that we’re all different and Twelve Step is one of many options. If it works for someone, great! But I feel like I was lied to. No one presented me other options and, so, the burden for failure fell on me in my ignorance.
The legal system, treatment industry, and media present a one-size-fits-all model that left me feeling worse. Judges mandated I attend Twelve Step meetings. Since every meeting starts with: “Rarely have we seen a person fail who has thoroughly followed our path,” I thought something was wrong with me since I kept “failing” by that program’s standards. A treatment system that pushes square pegs into round holes, then blames them for not fitting, is not conducive to success or healing.
Many people recover without treatment.1 Some can moderate their substance use. Twelve Step works for some. People with opioid use disorders have options, but they’re often denied to or hidden from us. Most rehabs, drug courts, prisons, and probation departments forbid access to medication-assisted treatment (MAT).
2. Forbidden Fruits: Methadone and Suboxone
MAT with methadone and Suboxone is the most effective tool we have for opioid use disorders. Manypeer-reviewed studies and consensus statements confirm its success at improving quality of life: treatment retention, reduced mortality, reduced crime, reduced jail time, reduced risk of disease transmission, improved health and self-care, and improvements in rebuilding vital relationships.
Therapists and self-appointed experts spent years telling me methadone is “legal heroin.” “It gets in your bones, rots your teeth.” “You’re trading one drug for another.” “The withdrawal is worse than heroin!” (Not true for me.) “Liquid handcuffs!”
Methadone liberated me. It saved my life. It stopped me waking up every day searching for ways to not be dope sick. I found much-needed medical and psychological care.
Where do these myths about MAT originate? What purpose do they serve? The CDC, NIH, and SAMHSA consider methadone treatment the “gold standard.” Why did this information fail to come up in my shuffle through support groups, the legal system, or inpatient and outpatient treatment? Even President Obama recognizes the value of replacement therapy: His three major proposals at the National Heroin Summit in Atlanta a few weeks ago mention MAT.
3. A Slip or Relapse Doesn’t Mean “Go Back to Start”
Learning that a slip or relapse doesn’t erase everything I’ve accomplished marked a shift in my thinking about substance use and recovery.
Like many others navigating their way through this system, I was taught that one slip erased my accumulated “clean time.” I had to come back and surrender when I “really wanted it” or “hit my bottom.” For many people, that bottom is death.
Now I don’t track “clean” time. In SMART I learned new ideas about the recovery process and stages of change. A slip is not a failure, but an opportunity to find new coping skills. Relapse isn’t a necessary part of the recovery process, although I’d been taught it was a defining characteristic of my “disease.” I learned skills to help me modify harmful behaviors. Instead of blaming myself, I learned healthy ways to cope with urges.2
4. I’m Not Powerless
I’m the only one capable of changing my behavior. My self-empowerment began with finding medical care which reduced the harms of using. In the early stages of MAT, I slipped when I thought I could sneak around a drug screen or stress became unmanageable. But the clinical setting transformed how I thought about drugs, gave me tools to reduce harmful effects if I did use, and put me on the path toward a healthy life.
Self-empowerment is absent from many treatment models. That’s changing as evidence-based practices become more mainstream. Despite stereotypes, most substance users are intelligent. When given the tools to succeed, we can. Telling me I’m powerless, then blaming me when I screw up, is demeaning and demoralizing. How can “experts” medicalize addiction, then deny us medication or punish us for relapse?
5. My Behaviors Don’t Define Me
I did some awful things while using drugs. Social stigma and the media’s portrayal of heroin users as “junkies” whose brains have been hijacked into only searching out our next fix, leads us to internalize negative attitudes.
From an early age, I compared myself to other people. When I wasn’t as smart, good at sports, or whatever else as the next guy, it banged up my self-esteem. We’re socialized to be competitive. That can be harmful.
During treatment I learned about Albert Ellis’ concept of unconditional self-acceptance (USA). Ellis was a pioneer in developing empowering psychotherapeutic models. SMART Recovery is influenced by his work.
USA means my behaviors, good or bad, don’t define me. I’m my own unique person first. It’s impossible to screw that up. “Bad” behaviors or mistakes don’t make me worse than anyone. “Good” behaviors or success don’t make me better. This liberated me from the myth of self-esteem and revealed my inherent value as a person.
6. People Use Substances for Reasons
My first dose of heroin produced what I imagine “normal” feels like for most people. A mentor of mine says, “people use drugs for reasons.” For me, heroin felt like necessary medicine. That’s why I kept taking it.
Before I ever touched drugs, my mental health was a wreck. I’d survived trauma, abuse, isolation, and a slew of undiagnosed mental health conditions. It would have been abnormal for me not to self-medicate. I sought mental health care, but every visit to the doctor ended with a prescription for a different antidepressant. I wasn’t depressed. The pills never helped. Within a year I was using heroin every day.
Heroin often comes with physical dependence, but that’s not why I kept using. I achieved periods of abstinence, but always returned because my brain was in distress. Even when I found success through methadone treatment, I believed the ultimate goal was complete abstinence. Same went for my later Suboxone treatment. My doctor (not a mental health or addiction specialist) pushed me to taper. That sent me into the worst bipolar cycle and roughest six months of my life.
Since then I’ve learned some people require medication indefinitely.3 In fact, for many people outcomes improve the longer patients are in treatment. Now I’m on an effective dose of medication, receiving mental health care, and am healthier than I’ve ever been.
7. Reality-Based Education
I grew up hearing: “Just Say No.” Schools presented panic-driven and exaggerated misinformation about drugs, with no mention of what to do when we find ourselves in trouble.
Recently I had the opportunity to hold an “anything goes” discussion with middle and high school students at a local alternative school. I was amazed that kids are still taught these outdated concepts and that many students know more about drugs than their teachers. This is inexcusable when we’ve learned so much about addiction in the last three decades; when reality-based resources are available for students and parents.
Students should not only learn the risks of substance use, but where to find treatment, how to use safely if they’re going to experiment (and we know they are), how to avoid HIV and hepatitis C, and who to talk to about trauma and physical or sexual abuse without feeling judged.
We have an opportunity to help future generations avoid obstacles that tripped us up. We need to own up to the fact that not only is the War on Drugs a failure, but so is our approach to drug education.
Carving Out a New Future
Now I’m a state-certified peer recovery specialist, a great honor and a tremendous accomplishment. I have the opportunity to help people navigate their own journeys to recovery—and sometimes intervene before that’s necessary.4
Long-term recovery from harmful substance use happens in communities. If drug users are exiled, incarcerated, pushed to the margins of society, they might never make it back. I’ve lost too many friends and seen too many people thrown into prison because we refuse to collectively confront flaws in our approach to substance use and recovery.
By placing compassion and honesty at the forefront, we can carve out a new path that creates spaces for people to heal, and empowers them with tools they can use to achieve a healthy lifestyle and determine the conditions of their recovery.5
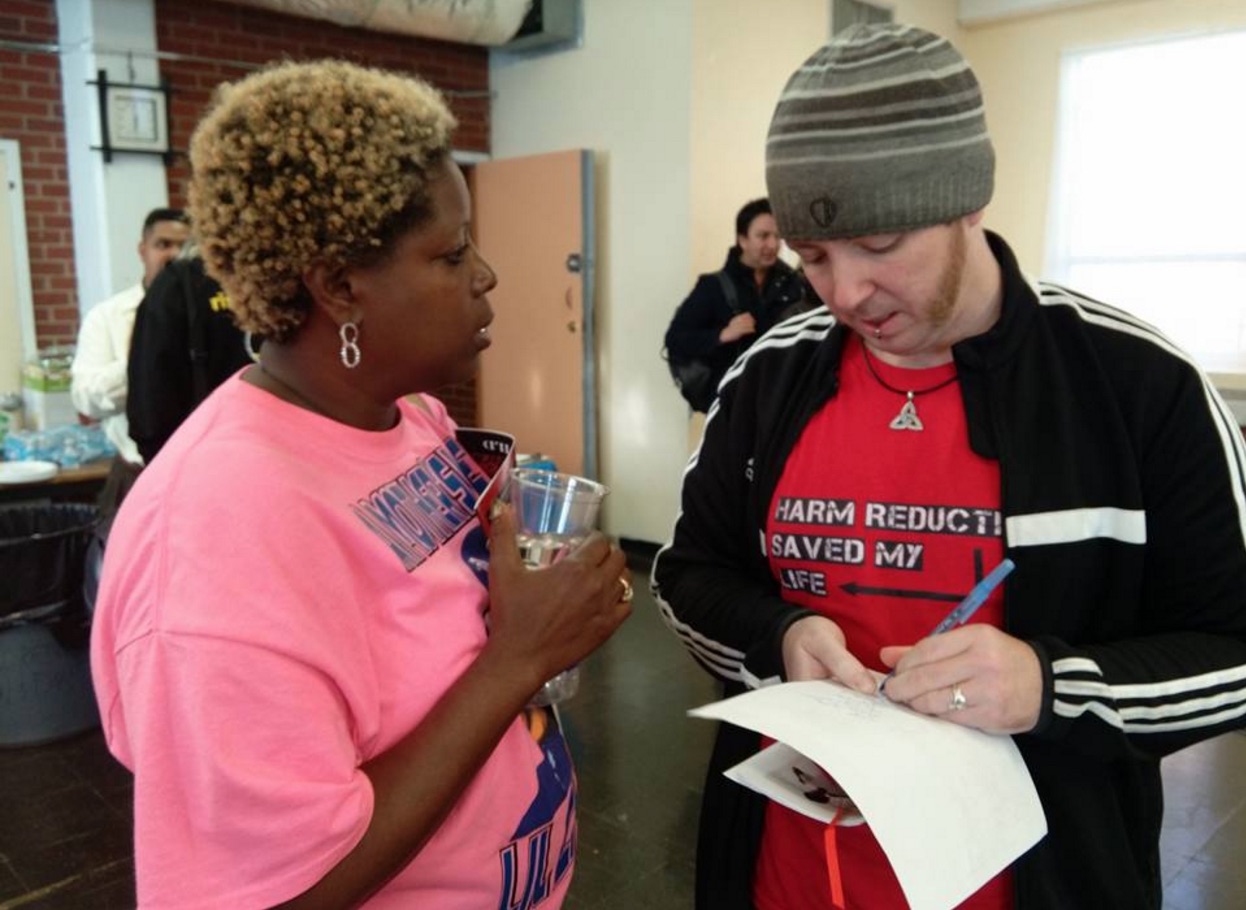
Jeremy is Harm Reduction Coordinator at Families for Sensible Drug Policy, Program Director at Southeast Harm Reduction Project, co-founder of Georgia Overdose Prevention, and a state-certified peer recovery specialist. He lives in North Georgia with his wife and 3 cats. He writes and speaks regionally about drug policy reform, harm reduction, and the importance of including voices of directly-impacted people in policy decisions.
Footnotes:
1. For more on natural recovery and “maturing out” of substance use, see:
A. Quitting Drugs: Quantitative and Qualitative Features, Annual Review of Clinical Psychology (2013), Gene M. Heyman;
B. Natural Recovery from Opiate Addiction: Some Social-Psychological Processes of Untreated Recovery, J. Drug Issues (1983), Dan Waldorf;
C. Natural Recovery from Cocaine Dependence, Psychology of Addictive Behaviors (1999), Toneatta, et al.
D. This short video on addiction from Kurzgestat, and an accompanying talk by Johann Hari.
2. SMART Recovery has an online library of self-directed tools and worksheets, and a comprehensive workbook. Meetings are led by trained facilitators, usually peers, and offer an online community and meetings for people with social phobias (like me). They also offer resources for friends of family.
3. See SAMHSA’s Treatment Improvement Protocol 43, pp. 101-117 for complete guidelines for managing the phases of MAT, including guidance on how to make decisions about medication tapering and maintenance.
4. SBIRT (Screening, Brief Intervention, and Referral to Treatment) is a powerful tool for prevention. The President also mentioned the importance of peer recovery support specialists in his Atlanta speech.
5. Those conditions might include reducing their substance use or reducing harmful effects to their health. Not everyone has the same goals and some people can moderate how much they use. We should support any positive change and prioritize healthier lifestyle choices over demanding complete (or immediate) abstinence.
