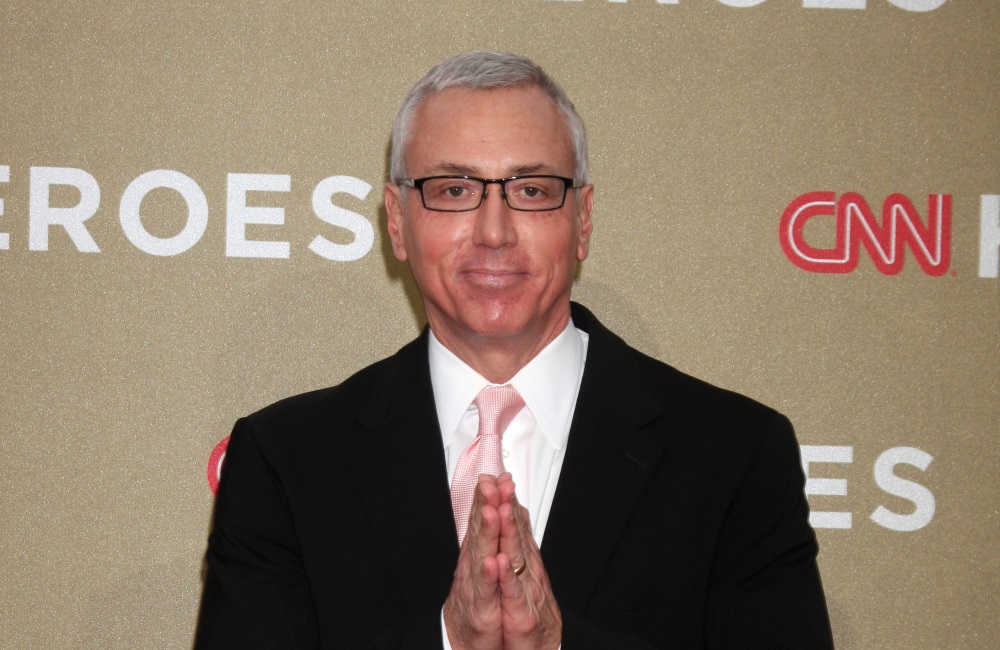
A practicing physician, Board Certified in Internal Medicine and Addiction Medicine, Dr. Drew Pinsky is an Assistant Clinical Professor of Psychiatry at the Keck USC School of Medicine. First gaining public recognition as the host of the nationally syndicated radio show Loveline, Pinsky later starred in the hit reality series Celebrity Rehab with Dr. Drew and the subsequent spinoffs.
A published author with several books to his credit, he takes pride in co-authoring the first academic study on celebrities and narcissism that evolved into the New York Times bestseller, The Mirror Effect: How Celebrity Narcissism Is Seducing America. Pinsky currently hosts the television show Dr. Drew On Call, in which he employs a therapeutic view on crimes and controversial issues in his analysis of current events. He lives in Pasadena with his wife Susan, and they have triplets who are now attending various universities.
In 2016, after 32 years on the air, Loveline ended a legendary run as a syndicated radio call-in show. It offered medical and relationship advice to listeners. What do you feel is the legacy of the show? What was the greatest moment for you personally, and how do you want the show to be remembered?
With a show that spans that much time, it’s hard to come up with a single moment. For me, I was always so grateful to have the opportunity to help young people. They would bring their material to us, and we got to hear in real time what they were contending with. I would hear about trends long before anything was put in the literature or even brought up by the press. If Loveline is remembered for anything, I’m always hoping that people will learn from the cases. When you go to medical school, you receive a certain amount of encyclopedic knowledge, but most of your training happens by listening to patients. That’s how you learn about the human experience.
Canadian addiction specialist Dr. Gabor Maté believes there is a strong link between early childhood trauma and later problems with addiction. Do you agree with this theory and do you think that it applies across the board?
Fundamentally, I agree. It’s complicated territory. What I have found is that if you have bad enough addiction, if your addiction is serious enough and complicated enough that you need to see me, there’s essentially a 100% chance that there was childhood trauma. Childhood trauma includes abandonment, neglect, sexual abuse, physical abuse, emotional abuse—interpersonal trauma is what we are talking about here. When that kind of trauma occurs, it is rocket fuel to the genetic potential for what we call addiction.
At the same time, there’s clearly a very prominent biological component to this disease as well. There also are other psychiatric and psychological issues that come to bear. Still, fundamentally, the problem that people are trying to solve with a substance is what we call affect disregulation, the inability to tolerate and regulate feeling states. Feelings are too prolonged, too intense, and too negative.
You have to then ask the question of, how does a human being develop a normal regulatory system? That’s something that we do in our interpersonal connections. Fundamentally, it’s the intimate connection that gives us the soil upon which two brains brought together can teach the mature brain how to regulate. It’s unfortunate when people have experiences that cause them to exit that frame. They usually are too vulnerable to be willing to reenter it. Then they start looking around for solutions, and the solutions in our culture include substance use, so, yes, there’s a very strong connection between childhood trauma and substance use.
The question then is, how do we go about treating it? The question of treatment gets even more controversial because the timing of when to deal with the trauma is not well studied. It’s been my experience that if you don’t get the substance use under control, if you don’t fully engage someone in either a 12-step type approach or some sort of therapeutic intervention for a sustained period of time before you really dig into the trauma, then you can do more harm than good.
If you dig into the trauma too early, then you can actually increase the probability of using. By highlighting the trauma, you can actually trigger a relapse. The pain of the trauma is so unregulated, and it’s so overwhelming for the person trying to recover to deal with the feelings associated with the trauma. They often abandon treatment and relapse to escape the pain. Today, we are relying more on a social model of treatment where people just learn how to live. They learn how to reengage with peers and how to redeploy intimate connection for affect regulation. Then, when they are ready, we start dealing more aggressively with the trauma. Does that make sense?
Yes, both from a big picture perspective and also because it parallels my own experience in recovery. When people are so broken in the early stages of recovery, dealing with the underlying trauma is not really possible.
What I usually do is show them the trauma, show them that all their peers have the same thing and that they’re not alone, then go, “That’s you. You experienced something similar, and it keeps you from trusting me. Let’s see if we can help you to tolerate some closeness and some trust so we can move forward.” I find that if I sort of paint the landscape for them, it helps them in the beginning.
Showing them the trauma early on makes sense in terms of showing people that they are not alone. It’s like the 12-step principle of identification. I had to learn early on as an addict that I was not terminally unique. In terms of being terminally unique, commenting on Prince’s death, you said early on, “Even if it ends up being drugs that caused him to stop breathing, I would put it more in the accident category than the addiction category. But still, an otherwise healthy middle-aged man with hip pain should not be on opiates chronically. Period.” Now we know that Prince was addicted to prescription opioids and died from a fentanyl overdose.
Similar to when Heath Ledger died of a prescription drug overdose, the celebration of Prince’s achievements seem to have pushed aside a moment when the dangers of drug abuse and addiction could be emphasized in a powerful and lasting fashion. Why would you initially put Prince’s death in the accident category rather than that of addiction? Shouldn’t such a high profile celebrity death be used to fight against the stigma and highlight the disease model?
Yes and yes. That’s my simple answer (laughing). You have to understand that my job is to try to assess things accurately. I still think that Prince is representative of another sub-category of a problem with substances that is a growing category. This is a little controversial, and I’m not even 100% clear on it myself, but I believe we are seeing a growing category of people who would not have developed addiction in their lifetime had they not been exposed to graduated and increasing doses of prescription opioids over time. In other words, I sort of put this in the category of drug dependency but not the full syndrome of addiction that we associate with the behavioral changes, the spiritual changes, and the inability to stop.
I believe that this category that Prince probably represented, although I don’t know because I wasn’t there, is a massively growing category of drug dependent people that look like addicts, but really are what we call iatrogenic addicts (iatrogenic means of or relating to an illness caused by medical examination or treatment). In other words, my peers, me and my peers, create these drug dependencies. These are not people that would be involved with substances had we not begun treating them and then continue to treat them over an extended period of time.
For instance, there is no underlying evidence that opiates are an effective treatment for chronic pain. Yet, my peers are treating people with high, escalating doses of opiates. Those are the patients that tend to go into that category—they lose control, and they die. We represent 5% of the population on Earth here in the United States, and we consume 80% of the opioids. I think there’s a problem.
Yes, and I believe Michael Botticelli as the head of the White House Office of National Drug Control Policy would agree with you as well. He has repeatedly seen the exact same things in his open forums across the country. The problem is not just in the streets, but on the prescribing pads as well.
It’s awful, an absolute catastrophe. The fact that it goes on breaks my heart. Some of these people certainly are addicts or become addicts. They would not have necessarily manifested the disease of addiction without being prescribed the opiates. We need to remind ourselves that each case of substance use needs to be evaluated individually. These are complex cases, every one of them. Each case has the potential to include pre-existing trauma issues, personality issues, psychiatric problems, brain injury from substances, withdrawal issues, post-acute withdrawal issues, iatrogenic issues, and genetic predispositions. Every case is a byzantine alchemy of all these different forces, and we really need to evaluate each one individually.
Personally, I have been completely sober for over eight years, and I have been clean from heroin and the opioids for well over twelve years.
Congratulations!
Thank you! The reason I bring it up is because I have a few lines in a poem I wrote about being addicted that goes, “The dopamine in my head is dead. / The superHIGHway under demolition. / Can I live again on a country road?”
Yes, that is what happens.
I know that was a major problem for me. In the same vein as you said earlier, opiates are like rocket fuel to the dopamine in the addict’s head. On a dopamine scale of one to ten, if four is the normal rate for triggering pleasure, the opiates shoot you up to a ten. As a result, once I got off the drugs, I felt practically nothing for the first six months to a year. The normal dopamine responses in my brain didn’t work. Until the balance was restored, everything seemed bland for quite some time.
Yes, that’s what happens to so many people in early recovery. The massive changes in the brain take a long time to come back and sometimes they never fully come back. It’s a very common response. It’s really common. Yes, it takes a while to come back, but to some extent, there have been permanent changes as well. Most people do not see the distinction between wanting and liking. With addiction, you want stuff that you don’t even like anymore. There is a difference in the brain chemistry between wanting and liking. After years of treating bad addicts, I have seen how the wanting takes over to the point where the liking no longer matters.
As an addiction specialist, can you explain the importance of having what you have described in the past as a “bullshit meter” when you are working with people with substance use disorders? Can you give us examples of how your bullshit meter has helped you in the past when it came to providing effective treatment to people with the disease of addiction?
My peers actually get offended when patients don’t tell them the truth. If my patients do tell me the truth, I become concerned that they don’t have the disease I’m supposed to be treating. Addicts lie. They lie all the time. It’s part of the condition. If you expect your patient to be honest, you don’t understand this disease and you don’t understand what is happening to your patients.
What I rely on is intuition. There’s something in the gut that you learn to trust. Rather than listen to what the patient is saying to discover the truth, you listen to your body and your thoughts and how you are feeling around your patients. You learn to read yourself and your own responses because patients do put out information that’s not verbal. You can attune yourself to this kind of information, and you can learn to read it effectively. It’s literally your body as an antenna.
Here is an example of how intuition figures into the process. I was doing an intervention with Steve Harvey, and the kid was refusing treatment. The professional interventionist had an intern with him, a young man a year or two into recovery. The kid we were trying to help bolted off into another room. I went over to the intern and said, “Come with me. I have a feeling that you’re going to be very useful.” I have no idea why I said that, except that my gut said, “Bring this kid. He can help.”
The intern entered the back room, and we left them there for about ten minutes. When they walked out of the room, everything was different. The patient had agreed to go to treatment. Later, as he was preparing to get on a plane and go to treatment, the kid said about the intern, “You know, it’s a funny thing when he came and spoke to me. My best friend had just died of a heroin overdose, and the words he was saying sounded so much like him, I thought he was actually speaking to me through him.”
Of course, when I heard that, the hair stands up on the back of your neck. I honestly see magical moments like that all the time in treatment. If you are open to those moments, they seem to happen quite regularly.
Right now, on a federal level in terms of the Obama administration’s response to the opioid epidemic, medication-assisted treatment (MAT) is being prioritized. Do you agree that MAT is the best way to address the problem? If you were in charge, what would you do in terms of addressing the opioid epidemic?
I know I would double down on the 12-step community by creating resources that would help people move in that direction. Some people say that there’s no research on 12-step recovery, and that’s simply not right. Of course there is. There’s research that compares it to every other form of treatment, and it has always proven to be as good as or superior to the others. And it’s free. In terms of efficiency and healthcare delivery, there’s nothing better than 12-step. That being said, however, there’s also a need for professional management. People have psychiatric issues and trauma issues, and these are very labor intensive, very expensive things to address. Naturally from the standpoint of the economics of healthcare delivery, a solution in a pill looks much better.
My concern is not the fact that medication-assisted treatment is being advocated, but rather my concern is the excessive enthusiasm for it. There’s no doubt in my mind that it saves lives, there’s no doubt in my mind that it’s an advancement, and there’s no doubt in my mind that for some carefully selected patients, it’s a critical ingredient in their care. It’s paramount. My concern is the profound, excessive enthusiasm for MAT and the deployment by people who really don’t understand addiction.
My next question is about how this drug epidemic is affecting families. In 2008, Barbara Theodosiou founded The Addict’s Mom as a small Facebook group with the slogan “Sharing Without Shame” as she struggled with the realization that two of her sons were drug addicts. Since then, with over 70,000 members nationwide, the group continues to fight against the stigma of addiction in the face of trying to save an addicted child. How do you think parents should handle the devastating weight of a child addicted in the family?
This is as complex, John, as dealing with the patient themselves. What I always tell people is that addiction is a disease that affects the whole family. Have you ever seen the movie The Little Shop of Horrors? Addiction is like the Audrey 2 plant that eats everybody that goes into the room—it’s a man-eating plant that demands to be fed. The Audrey 2 is a perfect model for the disease of addiction. It’s perfect because it never stops demanding to be fed, and, if you go near the plant, you’re going in the plant. Addiction functions and operates interpersonally. It infects interpersonal relations. If you’re with an addict, you’re part of the disease. No matter who you are, you become subject to the disease.
This is what family members like the mothers in The Addict’s Mom and other support groups around the country need to understand. This is why the 12-step program called Al-Anon has always provided such an essential resource. Everything that’s good about being a parent gets used and violated by the disease of addiction. You need to have the golden thread of Ariadne from the Greek myth to save yourself from the addiction. (In Greek mythology, Ariadne’s thread is what allows Theseus to survive and escape the labyrinth of the Minotaur). Dealing with an addict is like entering a dangerous labyrinth, and the person on the other end of the thread needs to have a profound understanding of addiction to help you navigate the dangers.
Ariadne’s thread is essential because addiction feeds on co-dependency. The very nature of the disease is to turn loving instincts against themselves. I understand this because I am a professional co-dependent, and my patients make fun of me. In the same way that addicts are always going to be addicts, I am always going to be a co-dependent. I have learned, however, how to manage it, how to turn it into an asset, but it also opens the door for treachery. You have to have someone there to help you with that challenge or you will get lost in the labyrinth of addiction.
In 2003, you authored Cracked: Life on the Edge in a Rehab Clinic, a book that recounted your experiences as the Medical Director of the Department of Chemical Dependency Services at the Las Encinas Hospital drug rehabilitation clinic in Pasadena. At the clinic, you treated the most severe cases of drug dependency and psychiatric breakdown. Can you discuss a couple of your most challenging cases? Can the pieces of shattered lives be put back together again?
The answer is sometimes. Many times. I obviously can’t discuss specific cases, but I can give you the broad strokes. Again, the magical part of treating severe addicts is that there are people I would not have given a prayer to recover that have recovered. There are people that I’ve actually kicked out of treatment who have walked up to me seven, ten years later—I can’t even recognize them because they look so healthy—and they’re sober and getting their PhD, often in psychology (Laughing). That happens a lot. It’s a very mysterious process, and I have seen some true miracles.
As for the kinds of tough cases that we would see, they often would have the trifecta—poly drug abuse, childhood trauma, and some sort of psychiatric problem. We would see these combinations of eating disorders, cutting, primitive personality disorder, borderline sociopathy and addiction. Unfortunately, these combinations of problems were not uncommon, frankly. They are quite common. It’s challenging to figure out which one is primary and which one to treat and which one requires the most attention. We would try to intuit our way through that while always trying to treat the addiction first. It was amazing how many times just treating the addiction ended up resolving so many things that looked like independent problems.
It’s so important to remind people during the beginning of their recovery and throughout the first year and beyond that it takes time. It’s such an important thing for them to remember. Let me emphasize something here. When you say it takes time, we’re talking years, more often than not. That’s the part that people lose track of when they look at what recovery is really all about. That’s where the 28-day model and the idea of fixing people in treatment falls way short.
I always tell my sponsees that the steps that haunt me long-term are the 6th and 7th steps about the character defects. The problem is that I relapse on my character defects on a daily basis. Even though I have been sober for many years, I still act like an alcoholic or an addict. When I put fear down on my list of character defects with my first sponsor, he shook his head and said, “No, John, they are all forms of fear. Fear is behind all of them. When you choose to side with fear as opposed to faith, your character defects come out as defense mechanisms.”
That’s a great insight. I would urge you, though, to always have good humor when it comes to the character defects. Those moments are often funny when you look at them, and some of our most tragic flaws also can be sources of great humor. When you are able to take a step back, you can learn from those moments. In working with patients, those times when they’ve been able to see themselves are magical because you can see the treatment working and the recovery starting to take hold.
In your eye-opening New York Times bestseller, The Mirror Effect, you look at how celebrity narcissism is seducing America. Given the profound changes blogging, tweeting, tabloids, and reality TV are having on the American way of life, how can parents protect their children? Has American popular culture become toxic, and what can be done to stem the rising tide and shift back to a healthier way of living?
Is it toxic? Yes, of course, and I think we can all readily see it. I think about this all the time, and I don’t know really what the answer is. I know what the solution is, but I don’t know how to get us there. Working a 12-step program, John, you’re going to know the solution as soon as I mention it. The solution is regaining a spiritual life, and a key component of that spiritual connection happens interpersonally.
We got to get back to us. We got to get back to families. We got to get back to love. We got to get back to connection. We have to re-prioritize the primary importance of the interpersonal. It’s hard to do because we are fighting essentially drugs, and I don’t mean chemicals. I mean the constant stimulations that our environment now gives us. It’s hard. We don’t even know the full effect on the next generation.
In a similar context, would you say that Celebrity Rehab with Dr. Drew, including the spinoffs Sex Rehab with Dr. Drew and Celebrity Rehab Presents Sober House, helped place the treatment industry in a positive light? Did it raise awareness in the consciousness of the general public about recovery? Do you believe it saved lives?
I want to believe that and I hope it did. It was our intention that it should. A week doesn’t go by that somebody doesn’t say to me that they went to treatment because they saw what we did, and it demystified or de-stigmatized the process of treatment, thus making it accessible to them. It was our intention, and you’ll understand that when I describe to you the way it happened.
Somebody approached me to do it, and I thought, “Ah, I don’t think so.” They kept expressing interest, and I kind of went into hiding. I just didn’t see it. As I was sort of hiding out, Bob Forrest, the guy with the hat and the glasses from the show, came into my office and said, “I am just so sick of seeing our patients ridiculed on television for being on a spa vacation when, in fact, they are in here doing treatment. I am sick of their hard work being diminished as something trivial. We need to do a TV show where we show how sick these patients are and how hard it is the work they do.”
I almost started laughing and said, “Funny you should say that because someone has approached me to do just that.” He simultaneously smacked both hands on his knees and he jumped up from the chair and stated with absolute conviction, “We have got to do this! We are going to do this!” Surprised by this burst of passion, I said, “Okay, if that’s your instinct, I’m going to go with it.”
On VH1, you served as the producer and starred in Celebrity Rehab and its spinoffs. There has been a lot of controversy about these shows because of the later deaths of several celebrity participants. Then again, people who go to rehab die from their disease on a pretty regular basis. Do you think these deaths have been overhyped to generate content for the pop cultural news machine?
People have very simplistic ways when it comes to headlines. This was a perfect headline to distill down in order to create a villain and make my team and I look bad. But you are right: If I did a show called Cancer House and people died, it would be expected and nobody would think anything of it. More than anything else, this reaction exposes how little people understand how dangerous the disease of addiction truly is. I treat bad addiction, and the probability of dying from it is higher than the vast majority of cancers today. Yet, if I did Cancer House and people died on the show, the reaction would be, “Oh that’s cancer. Of course they died.” The treatment would not be blamed. When I do addiction treatment, however, and somebody dies, my treatment failed.
You can’t treat them all, and people die under the best conditions. The other part that’s really hard for people to get their head around—and this is even hard for me as a co-dependent—is the patient has to participate in the treatment. This is the real conundrum of addiction. How do you get the patient to participate? That’s the hardest part. When they don’t participate, the outcomes are bad. If they do participate, miracles occur. But it’s hard to know who’s going to finally get it and who’s going to stay resistant.
Another tragic outcome that has particularly been highlighted by the opioid epidemic is how many times the people dying from overdoses are people who were trying to get clean. When they relapse, they go back and shoot up their old package, the dosage they were using before their tolerance was lowered in their effort to get clean, and they die. I have seen it over and over again.
What’s even scarier is that most of them today don’t even shoot the drugs. They just take medicines as prescribed, and they die. They take just a little bit more their benzodiazepines or sleeping medicines, and they die. Ninety-nine percent of the time now when my patients die, they die at the hands of my peers from prescription medication. They don’t die from overdosing on heroin and they don’t die from heart attacks from cocaine. They die from prescription medication.
This brings us back to my earlier point that is so crucial. If we just train and educate our physicians about addiction, then we can save so many lives. I have had people go in and say that they are an addict with back pain, and my peers hand them a benzo and an opiate. It’s insane because it’s like handing them a loaded gun. It’s even worse than handing them a loaded gun; it’s handing them a poison and telling them to take it. That’s how my patients die today, that’s when they die. Again, I must admit that it breaks my heart to see it happen.
Yes, it’s awful to see and experience firsthand, and I think that’s one reason why addiction has become such a national issue. Today, with the next presidential election cycle in full swing, Donald Trump is actually the Republican candidate. In the past, you have shown a real dissatisfaction with governmental overreach, taking an almost Libertarian political stance. What do you think this election says about the country in terms of its mental health?
You are asking me to comment in an area where I really don’t feel qualified, so let me preface my answer with the question: Who am I to make such a gigantic and leaping sociological conclusion? Having said that, yes, I do think that’s actually what’s happening (Laughing). Absolutely. This is my personal opinion.
But I still have a profound faith in the American people. It’s probably naïve, but we seem to have an uncanny way of finding our way out of not so happy moments and entrenched negative behaviors and biases. We have had a lot of trouble as a country, and we have done things that are not so great, but we seem to find our way out and to a better place. This is what I find remarkable. I just have faith in both the brilliance of the system and the ability of the American people to rebound from difficulties. I prefer to keep that naiveté because I honestly don’t know what is going to happen tomorrow. I do know what I see happening, and I do know that it makes me scared for us.
Let’s remove the word naïve and focus on the word faith. Do you think that faith comes from your father and his experience as the son of first-generation immigrants? Isn’t that faith a reflection of what some would describe as his immigrant spirit?
That’s a great question. I have never really considered it. I have been thinking a lot lately about the ethnographic things that are hidden from each of us. There are things that we do and that we are all engaged in, but we don’t really understand where they came from and why we are doing them. I have been thinking about that lately. Let me give that question some thought (Pauses).
I would say maybe not the faith when it comes to my father in terms of the classic definition of faith. My father had a deep faith in people. Like my father, I do believe this is a government of the people, and I do have his same faith in the people. I never thought that came from his immigrant experience, but from his clinical experience. He also was a doctor, and he really liked treating and helping his patients. There may have been something about his immigrant experience that contributed to that perspective. I was going to say that the immigrant experience that affected my family, I would put more under the heading of optimism and not of faith. But I do see how they are both there and they both are operating, but the faith I have is in people. The optimism I have is in people.
