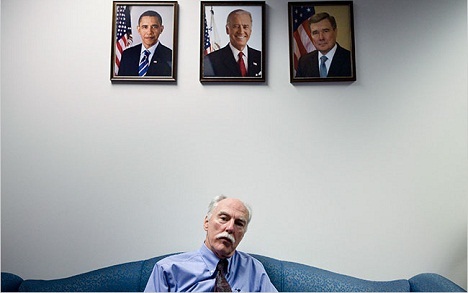
Candid and cantankerous, Dr. Thomas McLellan has never been one to sit still at meetings or tailor his rebellious opinions about addiction to please his audience. A Washington insider he ain’t, and damn proud of it, as he might say of himself. So McLellan was wary about heeding Vice President Joseph Biden’s personal call in 2009 to join the Obama administration as deputy drug czar. If one of his own sons hadn’t died of an intentional overdose of anti-anxiety meds and alcohol three months earlier even as another son was in residential treatment for alcoholism and cocaine addiction, he may have refused.
But facing the failure of the nation’s war on drugs in his very own home inspired McLellan to take a break from his job as professor of psychiatry at the University of Pennsylvania School of Medicine and scientific director of the Treatment Research Institute in Philadelphia. Equally persuasive was the fact that his boss, Drug Czar Gil Kerlikowske, the former Seattle police chief, had already announced that he was retiring the phrase “war on drugs” after 30 years because it implied that the government was doing battle against addicts themselves rather than the disease of addiction. It just so happens that McLellan has devoted his academic career to pioneering the disease model, doing as much as any other single individual to replace moralism with science in society’s view of alcoholism and drug addiction.
In the end, his stint as Washington insider was perhaps shorter than even he might have predicted. McLellan lasted only a year plus change—but it was a key year, with health-care reform (the Patient Protection and Affordable Care Act) on the move and the Mental Health Parity and Addiction Equity Act enacted in 2010.
Now back at Penn directing the new Penn Center for Substance Abuse Solutions, the folksy, moustachioed 62-year-old professor-activist is trying to get the private sector behind his campaign to treat substance abuse as a chronic illness. McLellan compares America’s too-little, too-late approach to the treatment of addiction—the “hitting bottom” scenario—to allowing a diabetic to lose a foot before addressing their diet.
He also argues that segregating substance abuse treatment from the rest of health care has scared away patients—not to mention funding for research to find solutions. But despite his cynicism about government, McLellan is remarkably hopeful that this entire failed system will begin to turn around now that health care reform and the Parity Act are law. Together, the two reforms are set to not only vastly increase medical coverage of mental health and substance abuse treatment but tie compensation of doctors and clinics to health outcomes rather than number of patients or services. More money, plus a new incentive for interventions that work, may set in motion far-reaching transformations.
I talked to McLellan over the phone while he wandered the streets of Honolulu between sessions at the annual American Psychiatric Association conference in May.
What do you mean when you say that addiction has been “segregated” from the rest of health care—and what exactly is the way out of that problem?
I don’t think segregation is unique to the addiction field. Other illnesses have moved from the periphery of mainstream health care into the middle—polio, TB, a lot of cancer, AIDS, depression, and now substance abuse. But when they’ve been segregated, a couple of things have happened: First, they’ve not gotten respect from the rest of health care, and, in turn, the patients who have gotten treatment have typically been the most complicated to treat—the sickest, those who really had no other choice.
Typically, a segregated illness moves into the mainstream only when there’s been political pressure or scientific discovery. New funding usually follows, and then a lot more people get treatment and they are a lot different from the people who have characterized the illness to that point. They’re much more likely to be earlier in the course of their illness, they have a far better prognosis—and that creates hope. As more people self-identify earlier, market forces and primary care take up the diseases and finally pharmaceutical firms say, “Oh, so it’s not just a couple thousand doctors who are going to prescribe our drug. It’s going to be 500,000 docs—good, that’s a market.” More drugs means more options, and so on.
McLellan compares America’s too-little, too-late approach to the treatment of addiction—the “hitting bottom” scenario—to allowing a diabetic to lose a foot before addressing their diet.
How far along is the treatment of addiction in the movement from segregation to mainstream?
We’re moving from an “addiction treatment” system to a “substance-use disorders intervention” system. And I think the reasons are political pressure—read the Mental Health and Addiction Parity Act—and also a lot of science. New medication, advances in neurology, all the interesting work in prevention have changed the atmosphere, and that creates opportunities to move into the center. And that’s what I think the Affordable Care Act—health care reform—will do.
In America, if you want to see real policy change, somebody’s gotta make a buck. There has to be something in it for somebody financially and it has to be sustained. One of the problems with the segregation of the substance abuse field is that we’ve carved out a very big market: There are 60 million people who drink or use substances in a harmful manner. Yet we’ve chosen instead to focus on the 2.5 million who are at the extreme end of the spectrum. I want to show businesses and local governments that they can actually save money by addressing all 60 million people through prevention and early intervention. If we can do that successfully, the forces of the marketplace will take over. All we lack is good ideas and preliminary data to show that it works.
Did you know that you needed a tablet computer a year or two ago? You did not. You never even imagined it. But in the first year they sold…what? 18 million iPads? Look out, marketplace.
How will the Affordable Care Act accelerate progress in the treatment of substance-use disorders?
Health care reform will have the first-ever primary-care benefit for substance-use disorders, which means it will be treated more like diabetes, for instance. Right now every insurance company offers diabetes counseling, assessment, diagnostic sessions and family counseling. Also home services, telemonitoring and a range of services to make sure people are doing well. The benefits are offered to 550,000 docs.
That has never been the case in the substance abuse world. The benefit has been only for addiction and only for either hospitals or recovery programs. So the care exclusively goes to people at the highest levels of severity—and by definition it cannot be individualized. Now substance abuse benefits will be very similar to diabetes care. So that’s going to help create a market for primary care doctors or nurses to try to manage substance use disorder.
People say primary care doctors and nurses can’t do it, they don’t know how, they’ve never been trained, they’ll screw it up. Yeah, I think that’s probably right, as a matter of fact. But they also didn’t do very well with depression, they didn’t do well with cancers or lots of other diseases. But the point is that the conditions will now incentivize learning and better methods.
And the kind of care that’s being suggested fits very nicely into the kind of care that’s being suggested for other chronic illnesses. Especially ones with big behavioral components—diabetes, hypertension, asthma, sleep disorders, chronic pain.
It’s not for me to make comments about AA because I’m not in recovery—I’m the only member of my family not. But peer support and of the AA variety could be useful for people who have not yet reached the point of no control.
Won’t the social stigma of being dependent on drugs or alcohol continue to set substance use issues apart from other illnesses?
My opinion is no. Take AIDS, for example. It’s tough to figure an illness that was more stigmatized. When AIDS was exemplified by homosexuals, IV-drug users, African-Americans and Haitians, it was impossible to imagine a more stigmatized condition. And what prevented that stigma from settling into real discrimination was the fact that they didn’t form separate, segregated AIDS treatment programs. Of course they had clinics, but it was integrated into infectious diseases and primary care medicine. And therefore you brought in a far greater range of people who were affected, and we began to treat HIV and not just AIDS. So that’s what I hope for with substance abuse.
I think there will continue to be stigma with substance use disorders, but the stigma will not be in having the illness but in not doing something about it. And in order for that to occur we’re going to need more options than we currently have.
Will the AA model of abstinence survive this transformation in substance-use treatment?
It’s not for me to make comments about AA because I’m not in recovery. In fact I’m the only member of my family not in recovery. But I think peer support and mutual support of the AA variety and others could be useful for people who have not yet reached the point of no control. Lots of people have found recovery without ever going to treatment. It could also be useful for the people who have done treatment and now need to sustain it. The best treatment program in the world is not going to be able to sustain sobriety unless the patient gets involved actively in something that’s going to change their lifestyle and sustain it. The estimate is for 20 million people, that’s been AA-style recovery. And that’s terrific. As good as it is, a lot of people don’t want it for whatever reason.
What about the role of harm reduction?
I think all kinds of harm reduction methods are very effective up to the point where you become really addicted. And I don’t know what that point is—as far as I know, nobody in science knows when that switch gets switched, but when that happens I don’t see you returning to the kind of lifestyle that you might have returned to at some prior point.
Do you expect there will be changes as well in the non-drug treatment of people with serious substance use problems? Rehab and AA both have such low success rates.
No, I don’t think there will be any effect on addiction treatment programs. I don’t think we’re going to see controlled drinking or drug use achieved, at least in my lifetime, for people who are at the top end of severity. Therefore, I don’t think we’re going to see fundamental changes in specialty treatment. I am one who believes wholeheartedly in abstinence orientation for specialty care. If you interview a thousand people, you’re going to find 30 who used to be addicted and now are drinking “normally” again, but it ain’t the way to bet.
Where I do think we’re going to see change—and again I draw on what’s happened with other illnesses—is at the earlier stages. We’ll see far more engaging kinds of individualized care that’s going to involve combinations of interesting therapies, self-help, mutual help, medications and social services. And they’re going to be offered in the context of other kinds of care.
Why are substance abuse disorders finally getting some attention at the national level?
Well, it’s not because doctors are looking for a new illness to treat or they’re so interested in substance abuse. And it’s not that the Affordable Care Act is sort of a bone thrown to the substance abuse field and uninsured people. Not at all.
The reason substance abuse is in the Affordable Care Act is because of the potential for savings in the rest of health care. It’s one of the biggest favors we’re ever gonna do for the rest of health care. You can’t treat chronic pain, sleep disorders, breast cancer, prostate cancer, diabetes, or asthma effectively or efficiently without simultaneous concurrent efforts to control substance use disorders. And it’s not necessarily addiction; it’s just people who drink too much, drink too often.
Take breast cancer. Most doctors aren’t aware that the amount of alcohol a woman drinks is a better predictor than the number of cigarettes she smokes for whether she gets breast cancer. And then once she gets breast cancer, any amount of alcohol accelerates tumor growth. If doctors want to treat breast cancer better—even if only for their own financial self-interest—they’re going to have to provide behavioral health care. And there’s no better predictor of what’s going to happen in medicine than appealing to self-interest.
How will people with substance abuse disorders experience these changes on a day-to-day basis?
It’s all going to be in the context of the “patient-centered medical home,” one of the centerpieces of the Affordable Care Act. This is basically team treatment. It’s designed around the team treatment of chronic illnesses. And it’s been designed to save primary care.
Primary care is falling faster than gowns on prom night. People are dropping out of it. Nobody wants to be a primary care doctor—they don’t make enough money and it’s way too much responsibility. So now teams of people will manage chronic illnesses using the electronic health record and patient registries. And one of the key members of those primary care teams is gonna be a behavioral health specialist. It’s not clear who that’s gonna be—a nurse, a counselor, a social worker?
If we just focused on depression, anxiety, sleep, weight and substance use—particularly alcohol and tobacco—we could vastly improve the course, the management, the outcomes and the costs of most other chronic illnesses. And that’s where you’re gonna see the real innovations.
Why did you decide to leave your job as deputy drug czar?
I didn’t like it. On a personality level it didn’t suit me. But I was proud of the White House Office of National Drug Control Policy, proud of the National Drug Control Strategy, and the part that I played in it. And no I’m not just being nice or politically correct.
But one of the most important factors for behavioral change in this country is the force of the marketplace. It’s second only to gravity in terms of how it changes behavior. And we really haven’t made much use of it. In my new center we’re working with three schools at the University of Pennsylvania: the School of Medicine, the Annenberg School for Communication, and the Wharton School of Business; we want to take the many good ideas out there—evidenced-based findings, protocols, whatever—and turn them into interventions that can be used by the public, by business, by schools, by government. I’m very excited about it.
If we were dealing in a field where I had a molecule and it was going to reduce pain better than opiates, I wouldn’t need to have my center because there’s already a vast pharmaceutical industry that takes those raw findings and turns them into drugs and then the force of the marketplace changes them. We don’t have that for policies, for social or behavioral interventions. And that’s what we’re trying to do.
Sally Chew was an editor at Time Inc.’s Health.com as well as at Vibe, Out and POZ magazines. She also authored a true crime book and was a wire-service reporter overseas. She also wrote about how to break out of a binge.
