Addiction is a complex, costly and debilitating condition. It exacts a heavy toll on individuals, families and society, and in this country that toll is even more acute because only a fraction of people ever get the help they need. The changes in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)—I chaired the DSM Substance-Related Disorders Work Group—signal a clear break from the field’s decades-old framework for identifying substance-related disorders. As beneficial as these changes will be for diagnosis, they also will have a positive impact on treatment.
This shift toward hard science is way overdue. Since the DSM was last published in 1994, brain imaging and other scientific advances have provided a greater understanding of the biological processes underlying addiction. We know much more about how alcohol, cocaine and other drugs activate certain areas of the brain and the neurological consequences. As a result, we now see addiction in terms of a continuum of symptoms and behaviors, not the artificial dichotomy imposed by the previous labels of “Substance Abuse” and “Substance Dependence.”
The DSM-5 resolves the longstanding debate over this abuse/dependence distinction. This debate has caused enormous confusion about the meaning of addiction among patients, the public and even clinicians.* Ending this debate is a significant accomplishment by the DSM-5.
The revision combines the dual classifications of abuse and dependence into a single category of “Substance Use Disorder.” It defines this overarching disorder as a spectrum of symptoms that go from “mild” to “moderate” to “severe,” and the criteria for each have not only been combined but strengthened. They require an additional symptom to be present for a “mild” diagnosis, compared to the current criteria for substance abuse. This evidence-based change actually raises the requirements from the DSM-IV without broadening them. Additionally, the DSM-5 criteria require that symptoms lead to clinically significant impairment or distress.
By removing the label of “dependence,” it also prevents the confusion when the appropriate prescription of psychoactive medications for pain, anxiety or depression results in tolerance and withdrawal and often causes the clinician to mislabel the patient as “dependent,” in the addiction sense of the word.
Critics say the new approach will divert resources from more serious patient cases. But that’s wrongheaded—early treatment will be faster, less costly, and more successful.
The cumulative effect of this redefinition, I believe, will advance treatment in critical ways. The characterization of the severity levels for these conditions, rather than the misguided distinction between abuse and dependence, has the potential to better direct the type and intensity of prevention and treatment services. It will inarguably improve the accuracy of treatment.
Let’s start with early intervention. We’ve long known that the earlier we interrupt the cycle of addiction, the better the likely outcome. In the process, we may minimize or prevent serious comorbidities. The severity scale that is integral to substance use disorder will help clinicians assess individuals who are in initial (“mild”) stages and focus on the most effective treatment for that point in time. This early intervention is expected to be a major public health benefit.
Such staging has not previously been used with addictions, and some critics suggest that it will divert resources from more serious patient cases. But that’s wrongheaded. Why wait to act until addicts are on the brink of requiring costly hospitalizations or even transplants? We need faster, less costly, and more successful interventions and treatments—and DSM-5 will position us for that. Our healthcare system saves $7 for every $1 spent on early care for substance use disorders, and that’s another value of the “spectrum” approach.
We also foresee marked gains in the area of pain management. We’ve all heard too many stories of patients suffering needlessly because either they or their doctors feared—incorrectly—that a prescription for codeine or other opiate-based drugs could be a prelude to future addiction. Their misconception stemmed, once again, from the DSM-IV’s unfortunate construct of substance dependence, which for many people became synonymous with addiction.
Yet studies have shown that dependence can be the body’s normal response to a chemical. Clinically, the word describes only physical symptoms, as evidence of increasing levels of tolerance, not any psychological response involving compulsive, pathological behavior. The latter, of course, is what’s key to actual addiction. We expect that the new unified approach to diagnosis will clarify the distinction. Tremendous harm has been done to some patients who have had legitimate, needed medication withheld. But no more, we hope.
As its diagnostic starting point, the DSM-5 addresses each specific substance as a separate disorder (“cannabis-use disorder,” “alcohol-use disorder,” etc.), with the severity of the disorder depending on how many symptoms a person has. Detractors continue to argue that the thresholds for diagnoses have been lowered and that that will lead to increases in prevalence. Their claim is hard to support based on numbers alone. Nearly a dozen symptoms now must be present for the most serious diagnosis.
In the Work Group’s due diligence, we looked at the impact these changes could have on the prevalence of substance use disorders. In a secondary analysis of data from 43,000 randomly selected Americans, no significant change in prevalence was indicated. Several smaller studies supported this finding.
Collectively, the definitions and criteria debuting in May with the new manual’s publication offer us a more comprehensive and multidimensional model of care for any substance use disorder. They represent essential progress in diagnosis, and I’m convinced that they will immediately begin to influence treatment. But they’re hardly the final word. For the sake of the millions of people struggling to overcome an addiction, we must push much further ahead.
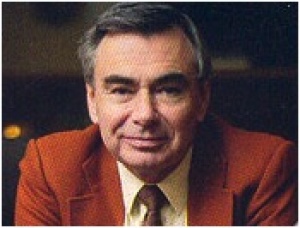
Charles O’Brien, MD, PhD, is a world-renowned specialist in addiction psychiatry. He served as the chair of the DSM Substance-Related Disorders Work Group for the DSM-5. He is the vice-chair of psychiatry at the University of Pennsylvania, and the director of its Center for Studies in Addiction. He was elected to the Institute of Medicine of the National Academy of Sciences in 1991, and has advised the US government on drug policy for decades.
*In 2006, Nora Volkow, MD, the director of the National Institute on Drug Abuse, T.K. Li, MD, then-head of the National Institute on Alcohol Abuse and Alcoholism, and O’Brien co-authored an editorial in the May American Journal of Psychiatry stating unequivocally that “experience over the past two decades has demonstrated that the decision [by the DSM-IV to include “dependence”] was a serious mistake.”
