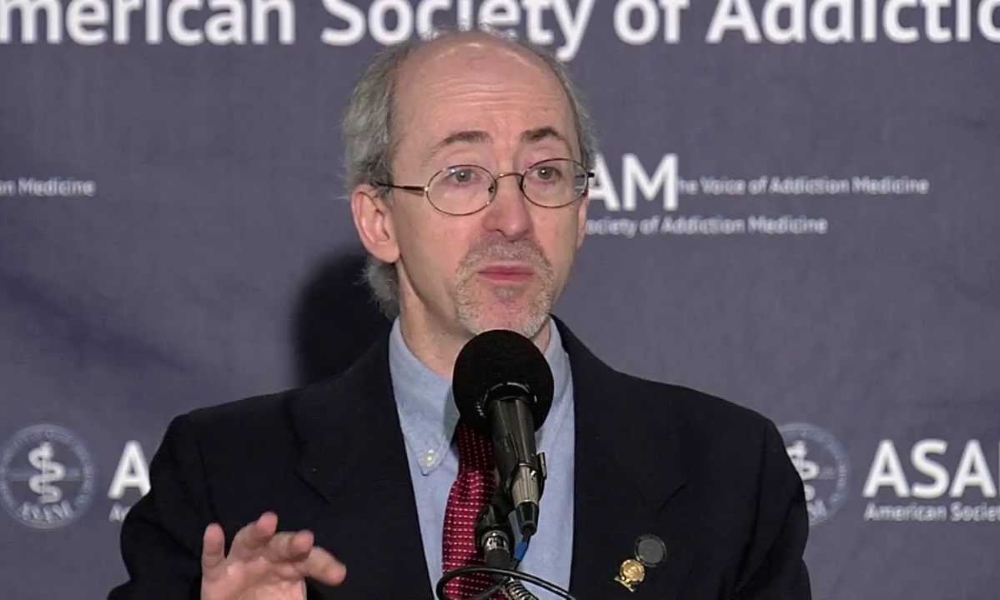
As the former President of the American Society of Addiction Medicine, Dr. Stuart Gitlow is one of the key voices today in the field of addiction treatment and recovery. As a general, forensic, and addiction psychiatrist, Dr. Gitlow is a noted expert on the delicate balance between the medical and the legal. As the executive director of the Annenberg Physician Training Program in Addictive Diseases at Mount Sinai School of Medicine, he helps to educate the next generation of doctors in the disease of addiction and the specific challenges in relation to delivering effective treatment.
Dr. Gitlow is a frequent contributor to textbooks about addiction medicine. In 2001, he published the book, Practical Guides in Psychiatry: Substance Use Disorders. Now dividing his time between his clinical practice in New England and his academic work in New York City, he is on faculty at both Dartmouth and Mount Sinai.
Can you tell us about the American Society of Addiction Medicine? What was the organization’s genesis, and what is its ongoing mission?
The American Society of Addiction Medicine was founded in the 1950s by a group of physicians based in the greater New York metropolitan area. ASAM has gradually grown to become national in scope. In the beginning, it largely focused on the treatment of addictive disease from a medical perspective. This was about the same time when alcohol was being accepted as a disease rather than a behavioral disorder. Along those same lines, the organization grew to become a membership organization of doctors specializing in the treatment of addictive disorders.
The ongoing mission is very similar to what the mission was in the beginning. The difference is that the organization largely focused on alcoholism in its earliest years. Today, it focuses on all addictive disease. The mission is the provision of appropriate care to those individuals who suffer from addiction, the overview of related public health matters, and the recognition of the addiction medicine physician as being part of a subspecialty in the field of medicine.
You are also the Executive Director of the Annenberg Physician Training Program in Addictive Disease, which you started in 2005 to ensure medical student access to addiction training. What have you been able to accomplish with this program?
The program itself began as a way of investigating and exploring methods that would allow students to maintain the degree of interest in the field of addiction that they have when they first enter medical school. Unfortunately, research has been pretty clear that when medical students first start med school—the first day of their first year of a four-year process—they believe addictive disease can be treated and they have an interest in treating it. By the end of their fourth year of medical school, they feel that addicts don’t do well with treatment, and they have lost their interest in entering the field. This is despite their being educated with respect to addictive disease in much the way they are educated about every other medical illness.
We set about to find different ways that the students could be stimulated, trained, and so forth, as a way to see whether new techniques, new methods, new educational approaches would result in an improvement of that research finding. What we found so far—it’s an ongoing research project—is that if students are placed in the midst of the epidemic, if they are placed with patients who have addictive disease, living besides them, learning besides them—much as the patient is learning about his or her own addiction—it leads the students to recognize that they and the persons with addictive disease are not very dissimilar. They have a lot in common. This allows them to identify with the individual and have more empathy for the individual than they do otherwise. It leads them to have greater interest in the field and greater knowledge about the patient with addiction. What we’re finding is that the more we can do to place students within that type of setting, the better the outcome.
That’s what we’re accomplishing so far. The next step, of course, is to try to figure out how we can implement such a plan of action. How can we make it happen for the students? It used to be, when we started the program 10 years ago, placing a student in a rehab and having them learn and grow beside a person with addictive disease. It used to be pretty straightforward. Now we run into liability issues, programs questioning whether or not there’s privacy and confidentiality, and all these regulatory issues come into play. Such issues tend not to be particularly meaningful in fact, but are very meaningful on paper. We’re struggling a bit to try to figure out how we can involve the medical students without stepping on the toes of the attorneys.
In 2001, you wrote Practical Guides in Psychiatry: Substance Use Disorders. Do you consider substance use disorder to be a disease of the brain?
As opposed to a disease of what else? [Laughs] I guess that would be my answer. Is it a disease of the brain as opposed to being a disease of the left thumb? Sure. I can’t imagine where else the disease might be but in the brain.
Clearly, once somebody has begun using addictive substances, they develop disorders of multiple organ systems. If you drink too much alcohol, you’ll develop a disorder of the liver, if you smoke tobacco, you develop pulmonary disease and so forth, but prior to the direct impact of the addictive substance or behavior itself, the disorder must be in the brain, if only through exclusion. There’s no place else that makes sense.
The brain is the organ system that determines to what extent learning impacts behavior. If I light a match under your finger, you learn that the fire will burn. The next time I light a match, you will pull your finger away in time to avoid being burned again. Yet, when an alcoholic drinks so much that they end up having a car accident, or their wife walks out on them, or they lose all their money, or their children end up hating them, they do not seem to learn from the experience. Rather than learning from the experience, they repeat the experience. They have failed to understand and make the connection necessary to do otherwise. The only place where that failure can take place is in the brain. Therefore, yes, it’s a disease of the brain.
That being said, it’s really a given at this point in time. It’s not as though I consider it that way as a matter of opinion. I think that for the past 50, 60, 70 years, the general knowledge and understanding of it has been as a disease of the brain. It’s sort of like asking me if I consider the world to be spherical. Yes, but it’s not a matter of opinion, it’s not because I’ve made a conscious decision to think of it that way, it’s simply because the world is, in fact, spherical.
How can psychiatry help battle addiction? Do you believe psychiatry is an essential component of addiction treatment?
It depends on how we look at psychiatry. ASAM was not founded by psychiatrists; ASAM was founded largely by internists. In fact, the majority of members of ASAM are not psychiatrists. Despite the fact that I am a psychiatrist from my primary training perspective, I am hard-pressed to look at it as an essential component if only because most people who treat addictive disease are not psychiatrists.
That doesn’t mean they are not using psychiatry. Psychiatry is the study of the mind and addictive disease is based in the mind because the mind is the brain. As a result, psychiatry comes into play. I’m not by any means saying that psychiatry is not an important component of addiction treatment. You don’t have to be a psychiatrist to treat an addict. It perhaps is a distinction that may not be necessary to make.
What I’m reading into this question is the following: Is there a psychotherapeutic approach that needs to be utilized in the treatment of addictive disease? The answer to that question is yes. Just as there is a psychotherapeutic approach to help people with eating disorders or high blood pressure or diabetes. We also have to talk to patients about being compliant with their medication or dieting correctly or exercising on a regular basis or getting the right amount of sleep each night. All of that is, at its heart, psychiatry.
Psychiatry comes into play with any chronic life-threatening illness to some extent. Addiction perhaps a little more than others because the disease happens to be brain-based. So I take it back; I said in the beginning that psychiatry is not an essential component of addiction treatment. I actually think it is an essential component. But one doesn’t have to be a psychiatrist to carry that out.
Being against the legalization of cannabis, you have stated that “people can … experience long-term psychiatric disease.” What kind of psychiatric disease is brought about by cannabis use?
Most of the recent literature has focused on the degree to which psychosis is initiated and maintained secondary to marijuana use. There used to be only this relationship that was understood. Individuals who used cannabis regularly seemed to have a higher rate of psychosis incidents than those who did not. Of course, one question that was asked was the following: Could it simply be that people who were going to become psychotic for some reason had a higher likelihood of using marijuana than other individuals? Maybe there was something else going on; some gene that crosses over that we don’t know about. Could it be that marijuana, in fact, is not causing people to become psychotic, but simply is being used by more people who were going to become psychotic than we would otherwise expect given the population figures?
More recent data seems to suggest pretty strongly that, in fact, it is the marijuana use itself that leads to a higher likelihood of a psychotic illness. Some recent data out of London in particular seems even stronger than what we have seen previously. It’s not a high number. Like all these addictive substances, the numbers are not in the majority. Tobacco does not kill most of the people who use tobacco. Alcohol does not cause damage to most of the people who use alcohol. Similarly, marijuana does not cause psychosis in anywhere near the majority of people who use the drug. In fact, the vast majority will not experience psychosis.
But about 1 in 100 will become psychotic as a result of their regular marijuana use. Although those odds for any one person are, I guess, pretty good, and, if I get one of my friends to use marijuana, he probably won’t become psychotic. But if I get 100 friends to smoke marijuana, one of them probably will. When we look at the public in general, we are looking at big numbers. As a result, we are starting to see as marijuana use increases, as people’s perception of its safety increases, we are starting to see some real scary numbers of individuals showing up with psychotic illness.
The other side of it is that you get a drop in cognitive status. That’s true in virtually all the people who use marijuana regularly. There is a decline in overall attention focus and processing speed. There again, if you have an individual who starts out with an IQ of 140, they probably won’t notice a significant change.
If you get the average individual that uses marijuana, however, which, according to the latest data, is an individual with a somewhat below average IQ to begin with, say they are starting out with a 95 now, after they have used marijuana daily for an ongoing period of time, they have dropped to say an 88. Right there, they have gone from being slightly below average intelligence to being right on the cusp of being unemployable. That’s a big difference. That kind of ongoing cognitive dysfunction and actual damage to the brain is what we really worry about in terms of public health.
It’s not like they are going to end up being hospitalized and it’s not like they are going to be treated. They aren’t going to come in and say, “Doc, I noticed that I can’t really read things as quickly as I used to and understand them.” They’re not going to come in, making that complaint. The damage to cognitive status is not going to be particularly obvious until long-term studies are produced, and that’s going to be quite a few years from now. It’s certainly obvious to those of us who treat the people who use marijuana regularly. You can tell the people who use marijuana before their backsides hit the chair in front of you simply because of the way they present themselves. Somewhat slower, somewhat more apathetic, somewhat more slow spoken, and that’s fairly typical.
But, again, if you start out with a very high functional level, you’re still going to have a very high functional level at the end of the day. It’s not going to make that impossible. But it’s not those people that we are focused on; It’s the average person that we’re worried about.
In Colorado, there is now everything from marijuana resorts to cannabis vending machines. Beyond the uses of medical marijuana, how dangerous is this public celebration of marijuana as an acceptable form of recreation?
First off, at ASAM and the AMA, we don’t see any such thing as medical marijuana. That’s a term used by the marijuana proponents. There’s never been marijuana, a plant that has been accepted by the medical community as having any value at all. Despite some legislatures claiming there is, but, the last time I checked, they weren’t made up of physicians to any significant extent. We don’t see that there is any use of marijuana as a medicine.
Skipping over that part of the question, the dangers of the public’s celebration of marijuana as an acceptable form of recreation are somewhat similar to the dangers of the public’s celebration of alcohol as an acceptable form of recreation. Back when prohibition was in place, we had a significant drop in per capita use of alcohol; about 50%. During that time, there was a 60-70% drop in alcohol-related disease. Cirrhosis dropped, fires dropped, accidents dropped. After prohibition ended, that public health success was thrown out the window. It took about 10 years for the per capita use to go up to where it had been pre-prohibition. Once that happened, of course, all of the fallout of the increased use of alcohol started to come back; the liver failures, the fires, the falls, the accidents, and so forth.
What we’re going to see with marijuana is the same thing. Prohibition ends, marijuana gets utilized as a recreational intoxicant, and marijuana has known toxicity and known negative impact that is going to affect the people using the drug. We will have a large portion of the public that is slower, less attentive, less focused, and processing information at a slower speed. We will have an increased number of people with psychotic illness. We will have a decreased overall public productivity and decreased revenue from taxes as a result of that. All of which will result from the public wanting another form of intoxication to be available to them; a drug that happens to be more dangerous than the other ones that are already available to them. But they don’t think that’s true so we’ll have to carry out this experiment live using the public and our children as the guinea pigs. That’s the way the public seems to want to take it.
Since as far back as the 1970s, marijuana has been called a gateway drug. From my own experience, marijuana definitely opened the door to my willingness to experiment with harder drugs. Do you believe this is the case today? Is it less or more so given the new legality of marijuana?
I don’t think any of the drugs are specifically gateway drugs. To some extent, you can look at the usual progression that somebody tries alcohol or tobacco first because they’re legal and that’s one issue that they’re not breaking or potentially breaking. From there, they may make the decision to do something else, usually while they are intoxicated to some degree, but not always.
But it is always a decision-making process. We surveyed medical students years ago, asking them which drugs they’d used and why they hadn’t used this one as opposed to that one and so forth. Many of their answers were very straightforward: “I never used marijuana or cocaine or heroin because they’re illegal. I used alcohol and tobacco because they were legal.” That was the deciding factor for a fairly large number of people. Then we asked this question as well: “If the drug had been legal, would you have been more likely to try it?” An awful lot of medical students said yes when asked that question. Legality was the specific factor they used when determining whether or not to try something. Now other people relied on other factors: “I’ve seen people have problems with it and I am not willing to take that chance.” Or “I’ve had a family member die of that and I would never try it.” Some people make the decision on another basis.
But any drug, once you have made the decision in your head, “Yes, I am going to take that risk because of the potential benefit of the intoxicating period,” then the drug will be taken. Because that’s the only benefit, right, the intoxication. The only possible benefit one gets from marijuana is the intoxication. If you are seeking that intoxication and you are willing to seek it, despite the known risks, and you make that decision once, it becomes easier to make that decision a second time, even with a drug that might have somewhat greater risks. In part, that’s because the drugs with greater risks have greater potential benefits, meaning more intense intoxication. Why might you try heroin or cocaine after trying marijuana? It’s simply because the intoxication is supposedly better, even if the risk is potentially higher.
In that sense, drugs can be a gateway. You’ve made one decision. It’s sort of like a decision that one makes when swimming. I will dive off the low board. Well, I was successful there so I will now dive off the middle height board. All right, that was successful, now I’ll dive off the high board. It doesn’t mean the high board is any less dangerous than it was in the first place. It’s easier to make the decision once you’ve already gone off the low and medium height boards. That’s all that’s happening here. I don’t call it a gateway, but there is a decision-making process in which marijuana will fall in the same way as tobacco and alcohol. From that perspective, the big gateway drugs are going to be tobacco and alcohol.
You did a forensic psychiatry fellowship at Harvard University. Can you illuminate what forensic psychiatry is and the role it plays in addiction research?
Forensic psychiatry is a subspecialty of psychiatry rather like addiction or geriatrics or child psychiatrist. A forensic psychiatrist deals with any issue at the crossroads of medicine and the law. For instance, if I ask the question, “Does this 70-year-old man who’s demented have the capacity to write a will?” I am asking a legal question that involves a medical determination. If I ask the question, “Should this fellow who killed somebody while intoxicated with cocaine be found criminally responsible for his actions?” That’s one of those legal questions that involves psychiatric input. Legal matters often will involve a medical issue, typically where the use of substances is involved and a civil or criminal act has been committed.
In terms of addiction research, we are getting a lot of driving while intoxicated cases where someone who tested positive for marijuana was involved in a motor vehicle accident. The question being examined by current research is to what degree did the marijuana contribute to the driver being in the accident? It’s a difficult question because the level of intoxication for marijuana may not necessarily correlate very well with the blood level of THC. Definitely not in the same way that it does with alcohol. As a result, a good deal of research is taking place to help establish those correlations.
You have twice sought election to the Rhode Island General Assembly. Is your interest in a political career connected to a desire to change public policy in relation to addiction and recovery issues?
I ran as sort of an outsider, I was new to the area, and I ran against a well-known incumbent. My expectation was not to win, but it did give me a sort of pulpit from which to talk about health-related issues that I felt were being largely ignored in my home state. It was a good opportunity to speak with members of the legislature and to access members of the media. At the time, the focus was the public debate over the Affordable Care Act. It was fun to be able to address some public health-related issues, but we certainly did address some addiction issues as well because marijuana was starting to become a hot topic as well.
You said that excessive use of video and online games, a problem that affects about 10% of players, should not be considered a mental illness. You clearly stated, “There is nothing here to suggest that this is a complex physiological disease state akin to alcoholism or other substance abuse disorders, and it doesn’t get to have the word addiction attached to it.” Do you still believe this to be true and, if so, why?
I might modify it a little bit, but frankly the human brain is constructed in a way where we naturally tend to repeat behaviors that we find to be beneficial. That’s where things go wrong with addictive disease. There’s nothing beneficial about the ongoing use of an addictive substance when everything in your world starts to fall apart. Yet, you repeat the use of it anyway. But it’s very difficult to distinguish that from the regular function of the brain, which is to repeat behaviors, which are beneficial.
If I really enjoy football and I go out and play football every day with my friends and I watch football on TV and I follow football in the sports pages of the newspapers and I poster my walls with pictures of football players and I believe football is just the best thing in the world and I go to the Super Bowl each year, I’m filling my life with football-related things, but do I have a disease? The answer is no because it seems to be within the range of normal functioning. If I go out to my garage every night and work on my old car, and that’s what I do every single night, and I spend hours and hours and lots of my expendable money on rebuilding that old car, I don’t have a disease. That’s what a lot of people do every day.
In fact, if you look at most people, they have an activity that they pursue to some degree to the point of excess. That’s the way the brain is constructed. It’s designed for us to do those things. The disease aspect of addiction comes into play when a substance or behavior has been demonstrated to have negative results and yet the person continues to do it. You gamble, but you lose all your money, and you do so repetitively to the point where you’ve lost your home and your family and your friends, yet you keep doing it. It’s a negative result with repeated action.
With video games, it’s tough. It’s very difficult to demonstrate the negative outcome with any significant percentage of people supposedly addicted. There are some that have a negative outcome, but it’s not the same as the other truly addictive disorders like gambling or compulsive eating or cocaine or alcoholism. Video game addiction could be generalized into obsessive-compulsive disorder or some other category of mental illness.
Then again, really, we are just talking about terminology. Once we figure out the genetic underpinnings of these illnesses, we’ll be much better able to answer the question as to which family they fall into and how they should be classified. It’s not that it’s an unimportant question, it’s not that we wouldn’t want to treat somebody who has experienced a negative impact of any activity, but it becomes a matter of whether we want to look at the brain as it functions for almost everyone as being addictive in nature, or whether we want to look at addiction as a mental disorder that negatively impacts a wide range of individuals that really need help.
With the “National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use,” is ASAM moving away from an abstinence-based focus in order to embrace harm-reduction techniques, both in treatment and long-term recovery as well?
We never had an abstinence-based focus. ASAM’s perspective has always been to follow the science. Whatever the science demonstrates as being an appropriate form of treatment for a disease, and that encompasses biological, psychological, sociological, spiritual; you name it. It’s all included. Whatever the science demonstrates as leading to the best possible outcome is what we’re going to promote and embrace.
If we were looking at diabetics prior to insulin, we would have said that we’re an abstinence-based treatment model. Once insulin gets introduced, now we’re a harm-reduction model. It’s sort of silly to isolate the use of medication as being some totally new approach. It’s not. We’re going to use whatever tools are made available that are demonstrated to result in a decrease in overall functional impairment and an improvement in morbidity and mortality figures.
The treatment of addiction involving opiate use involves the use of medications as a way of obtaining a better outcome. That’s the important part and not that it’s a harm-reduction model because it’s not really. It’s a model that simply results in improved function of the individual patient. A harm-reduction technique to me is making sure that clean needles are available to individuals that are using street heroin. A harm-reduction model would be the availability of high-grade heroin so that people who are going to use heroin don’t use street heroin that’s been mixed with God knows what. Those are harm-reduction approaches. What we are talking about is the effective medical treatment and medical treatment involves medications where the medications are demonstrated to lead to improved outcomes as they have been with opioid use disorders.
When you were asked in an interview, “What constitutes solid recovery?” for a patient, you replied, “Do they have an AA sponsor? Do they have a good AA home group, that is, a meeting that they are going to repetitively and have gotten to know the people there well? Are they participating actively in their recovery and taking responsibility for their illness?” Recently, there has been one of the periodic backlashes against 12-step programs. Do you still see 12-step programs as being an essential component to successful recovery?
That was only part of my reply and it happened to be the only part that was quoted. If I were to be asked now what constitutes solid recovery, I would say an individual who is demonstrating both abstinence from the original behavior or use combined with improvement in function. Are they back at work? Are they back with their spouse? Are they in a productive relationship with an employer or with their educational institution?
All of those things are key factors in determining whether or not somebody is doing better. I want them to not show active signs of their disease, meaning I want them not to be repeating behaviors that just get them in trouble. I want them to show evidence of improvement, and I want them to have some methodology of achieving this in an ongoing manner that includes that they’re being safe from stressors that might arise at some point in the future.
The time when people relapse is usually related to a key event; a spouse dies, the house burns down, they get fired from work for some arbitrary reason. Such people will often be at risk for relapse unless they are actively engaged in a recovery program. That’s where I want the recovery program to come in. I want the recovery program to come in not just to help get them thinking in the right direction initially, but to be a safety net for them. When something inevitably goes wrong as it does in everybody’s life, they will know who to call and how to speak to that person in order to make the choices that are not going to be destructive to them going forward.
What’s wrong in addictive disease is a failure of an individual to make the right decisions without thinking about it. These people make bad decisions routinely. If you make a bad decision routinely, then you are bound to make a bad decision in the face of disaster. Addicts often are in that situation where the decisions they make are bad if they don’t vet them with somebody. The 12-step groups exist, in some ways, as a vetting group. When something bad happens, you can call your sponsor and say, “This just happened. What do I do?” What to do: Go to a meeting, come on over, let’s go out for coffee, let’s make it so we can discuss this and you can make a good decision in regards to what to do in terms of going forward that makes sense.
That’s such a better outcome than picking up and relapsing. It’s probably going to be your first thought even if you’ve been in recovery for 20 years. That’s the disease of addiction. And that’s why meetings and 12-step programs are so important. From that perspective, I see it as being an essential component of successful long-term recovery.
John Lavitt is the Treatment Professional News Editor at The Fix. He last interviewed SAMHSA’s Frances Harding.
