Dr. Peter Grinspoon is a successful primary care physician in the Boston area, but it’s been a long road for him to get back to that point. He discovered prescription drugs while in medical school and was fully addicted by the time he had established his own practice. In 2005, he was arrested at his office for writing Vicodin prescriptions for his own use in the name of a former nanny. Grinspoon had his medical license and teaching position suspended, and faced three felony charges of fraudulently obtaining a controlled substance.
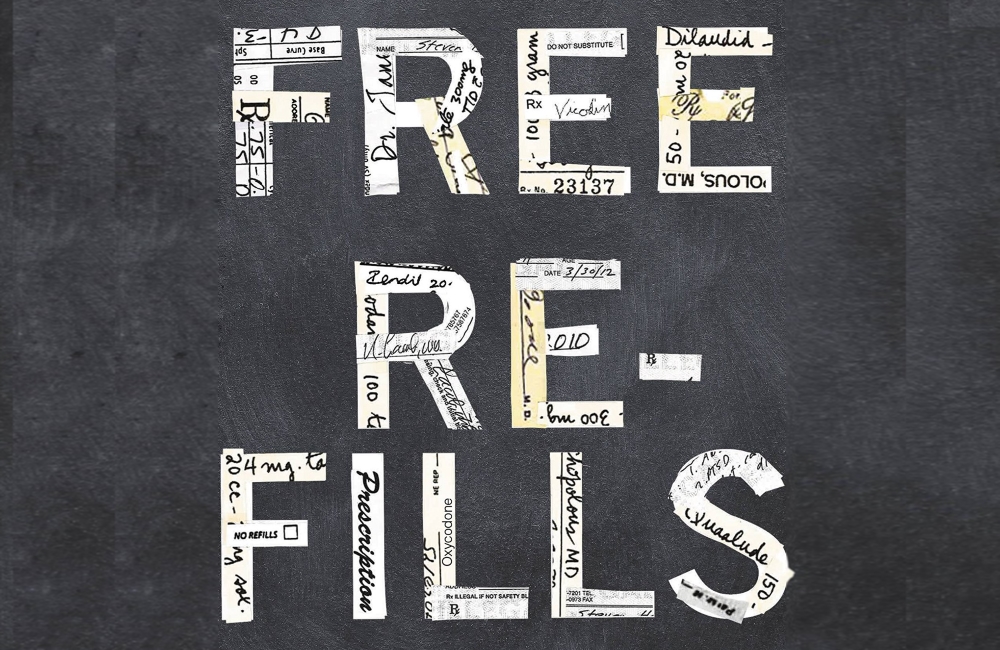
But when Grinspoon entered treatment and discovered other addicted doctors at the same facility, he was shocked to realize he wasn’t the only one. Now sober for nine years, working as a primary care physician at an inner city clinic in Boston and teaching medicine at Harvard Medical School, he’s finally ready to share the struggle of many addicted physicians in the U.S. His new memoir, Free Refills, chronicles his own recovery journey and his goal of reforming the current medical system to make it easier for other doctors to get help.
Grinspoon spoke exclusively with The Fix about the struggle to regain his career after his suspension, why many doctors are reluctant to seek help for their addictions and how current medical board policies are more damaging than helpful for doctors who need treatment.
Were there any concerns related to your career about releasing a book that goes into such detail about your former drug use?
There was absolutely a concern. It’s very possible that some of my patients will dump me. But nine years ago is a really long time and I’ve been back at work for eight years. And with the raging opiate epidemic among us now, this seemed like the right time to release the book.
When did your drug use first begin?
I smoked pot all the time when I was a teenager, but didn’t really get into trouble until I first tried opiates. And when I tried Vicodin in medical school, from that point on, part of my brain was committed to finding more opiates to take.
Personally, there’s no way I’d be able to finish medical school while also dealing with an addiction. How were you able to remain so successful in your career for a long stretch of time?
It did take a while for the addiction to gain momentum. When I was in medical school, I still took it sporadically. But as I moved into residency and eventually my practice, it became an everyday thing. I never took it before seeing patients and was never impaired at work, but was taking it every night towards the end and would be sick if I didn’t take it.
But I’ve always had a really strong work ethic. And they say with physicians and addiction that your career is the last thing that goes. You can still be in denial because you’re a successful physician. It provides you cover because nobody expects you to be addicted. And it certainly provides you access and resources to opiates.
The fact that I was a successful doctor really protected my addiction, but it’s interesting that these two things were not mutually exclusive. I was really motivated to be a good doctor and also really motivated to take opiates, but these two things never interfered with each other until 2005, when the state police and DEA came into my office. Then it definitely interfered [laughs].
Was that the moment when you knew something had to change or did it take more time after that?
The moment was sort of building up. Part of my brain was in complete denial. One of my therapists, who is an addiction psychiatrist, said I had more denial than any other client he had ever worked with.
But it was also hard to ignore the warning signs. There were days when I was really sick at work and my marriage was disintegrating. I was stealing pills and obviously knew that was wrong, but I was addicted so I did it anyway. I had a dawning awareness that this was no longer in my control and was going to do terrible things to my life, but at the same time, being addicted sort of controls your decision making. It wasn’t enough to get me to stop taking the pills.
When you went into rehab and saw that there were other addicted doctors in the facility, was it a surprise for you?
Absolutely. It felt like I was the only one. When I got caught, one of the first things that happened was that I was introduced to Physician Health Services, which is the physician health program in Massachusetts. They monitor you, drug test you and force you into support group meetings. I started going to physician and dental support group meetings pretty early on after getting busted.
And then I started realizing the extent of the problem with health care providers because there are lots of people like me. The rates of addiction in the general population are roughly estimated at 9%, but among physicians it’s about 10-15%. But certainly in the beginning, you feel like you’re the biggest screw-up on the planet and that you’re the only person who ever got themselves into this.
What were some of the consequences you faced legally and professionally in trying to rebuild your career?
I lost my job, for one. I had a “voluntary” agreement with the board not to practice medicine, which was essentially a suspension. I needed an active act from the board to begin practicing again, so I was definitely on the sidelines for a while, professionally. I had three felony charges hanging over my head for fraudulently obtaining a controlled substance, but ended up on supervised legal probation for two years and had to meet with a probation officer at least monthly.
Personally, my marriage was falling apart. I wasn’t making any money and then was hemorrhaging it from all the legal fees. And all during this time, I was trying to adjust to life without my main crutch of opiates. Early recovery can be a very dark time. It really felt like I was getting it from all directions.
There’s a belief among many medical professionals that getting help would be a professional death sentence. Was that a concern for you as well?
Absolutely. I think the best thing you can do for patient safety is make things less punitive for physicians receiving help. It’s so punitive now that you can get your license and livelihood taken away. A lot of people who are struggling don’t get help and are hiding in the shadows. The best thing you can do is to create an environment where doctors can openly say, “I have a problem. I need help with this,” and not fear losing their license. It was an obstacle to my care and I’m sure it is for a lot of other physicians who need help.
Is there a way for doctors to receive help without fear with the system as it currently is?
If you take time off, you have to explain it to the board. We’re not allowed to just take it, which I think is unfair. The one ray of hope is that in theory, the physician health programs are diversionary. That means if you’re having a problem with drugs and alcohol and you go to the physician health program, do their drug tests, sign their contracts, go to their meetings and be monitored for five years, in theory, the board is not supposed to find out about it.
But a lot of people criticize the program because it’s burdensome, expensive, and you get reported to the board for even a small misstep. Sometimes that misstep isn’t even your fault, like someone else not turning in your paperwork. But in reality, most physicians don’t trust that pathway and don’t trust that the board won’t find out about it. I think we have a long way to go until people feel like they can get help without the risk of severe punishment.
When you see patients who show signs of prescription drug abuse or doctor shopping, does it affect you more personally than it did in the past?
In some ways, I’m much better at picking out the scams than I was before because I’ve perpetuated some of those scams to obtain narcotics. As they say, you can’t bullshit a bullshitter. But at the same time, I feel a lot more compassion and empathy for the addicts I treat.
It’s difficult to get people into treatment because a lot of them aren’t ready, and I can’t force them as their primary care doctor. And because we’ve had this War on Drugs and been so focused on punishing people instead of treating them, there’s now a paucity of treatment options available and a lot of them are expensive. My primary care office recently sent someone to rehab and they couldn’t afford it. We are somewhat hand-strung in treating addicts.
What are some of the things that have worked for you in remaining sober?
Exercise really helped because it stimulated some of the same endorphins. Support meetings have been a huge help as well. But I think the biggest thing was having so much to lose and so much to fight for. If I didn’t get it together, I would never be a primary care doctor again, and that was my life goal.
When you’re in early recovery and feeling lonely or excited or whatever else, your first response is to grab a drug. But as time goes on, it just isn’t on the menu of options anymore. It becomes a habit and becomes easier.
