We’ve all seen the cliché movie script: squalid drug user decides to get clean, goes to a few meetings that start with “Hi, I’m John and I’m an addict,” and later graduates shining, polished, and ready to start a drug-free life. These stories are heart-warming, redemptive and, in true Hollywood style, total bullshit.
The drug treatment system in the United States has many dirty secrets, not the least of which is that it is far more difficult to access than most people realize. Even drug users themselves don’t know how near-impossible it can be to check into treatment until they try, only to hear: “I’m sorry, I see you have a domestic violence conviction from five years ago. You’re ineligible for treatment here,” or “I’m sorry, you take Xanax to manage your depression? We don’t accept clients with mental health issues,” or “Sorry, you’re 17. We don’t treat minors.”
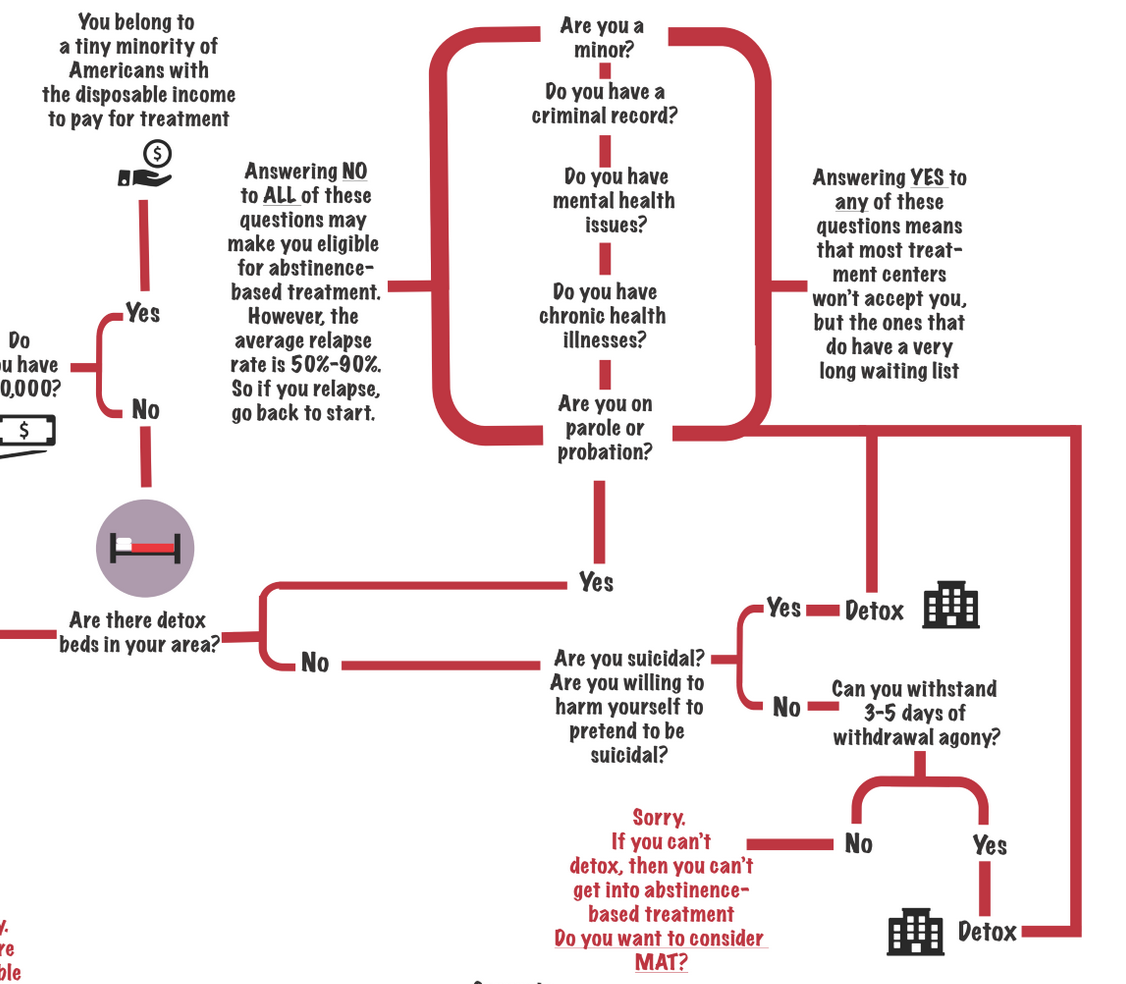
Numerous rules and eligibility restrictions exist that keep people who desperately need and want treatment from getting it. The following is a list of common catch 22s:
If you want to go to a private, residential treatment center, you won’t be able to work. But if you don’t work, you probably won’t be able to afford treatment.
Most people are unaware that the average private, residential treatment center costs $25,000-$30,000 a month. Sticker shock? Your insurance company probably thinks so too, which is why they will typically cover only 2-4 weeks of treatment (the recommended time for sustainable results is 6-12 months) and may require you to pay first and then apply for reimbursement. Additionally, since you won’t be able to work during the time you are in residential treatment, and most people’s insurance is tied to employment, once you give up your job to enroll in treatment you will lose your insurance anyways.
If you are among the 99.9% of Americans who don’t have $30,000 a month to burn, there are some government-run or non-profit treatment centers available that offer services for free or on a sliding scale fee. Some of these programs may require you to get a job and contribute financially as part of the treatment. Unfortunately there are very few of these around, particularly in rural areas that lack most social services in general. Also, if you are lucky enough to live in an area with a treatment program like this, you will probably be put on a waiting list for weeks, months, or even years. For many people, by the time the call comes to say a space has opened up, it is too late.
Click image to see the full-sized flow chart/ graphic courtesy of Hyun Namkoong
Many people with mental health problems use drugs to self-medicate. However, seeking professional help for mental health conditions can make you ineligible for substance use treatment.
According to the National Survey on Drug User Health, over half of people with substance use disorders have a mental health problem, often as commonplace as depression or anxiety, and they use drugs to self-medicate. Unfortunately, most of the free or sliding scale treatment centers don’t have the budget to hire staff members who are trained to handle mental health issues, so they turn away potential clients with mental health conditions. The kicker is that the only way a treatment center would know if you had a traceable “history” of mental health disorders is if you had attempted to seek help before. By soliciting professional help for a mental health issue, you create a paper trail that may block you from getting substance use treatment at certain facilities. A mental health condition is one of the top reasons a person would use drugs. It is also one of the top reasons a person would be turned away from treatment.
It’s hard to break the cycle of crime if you have an addiction, but it’s hard to get addiction treatment if you’ve committed a crime.
Because drugs are illegal, most people who have spent years in active addiction have a criminal record of some kind. In fact, according to the U.S. Bureau of Justice Statistics, 80% of incarcerated people abuse drugs or alcohol, nearly 50% are considered clinically addicted, and approximately 60% tested positive for drugs at the time of arrest. However, many treatment centers will not accept any patients with a criminal history, including people with an open court case or who may be on probation or parole. (Interestingly, many people on probation or parole are required to be in treatment, yet are ineligible for enrollment in all but a few specialized programs). Take the case of Misti Barrickman, a heroin user in Seattle, Washington. In order to be eligible to receive drug treatment, she had to go at least a year without an arrest or conviction. But because she was homeless, she had frequent run-ins with police, and each incident kicked her back to the beginning of the one-year waiting period. It was not until she was put into a diversion program that placed her in treatment despite the one-year rule that she was finally able to get help.
Most people who become addicted to drugs start using as teenagers. But in many areas of the United States, drug treatment is not available to minors.
One of the gaping holes in the U.S. drug treatment system involves recovery programs for minors. To use a typical example, Trinlie Yeaman of Asheville, North Carolina, spent a year searching for treatment options for her 17-year-old daughter, Zoë, who was addicted to heroin. Trinlie cried and pleaded with treatment centers, courts, hospitals, and social services, but was turned away at each one because no one would accept a minor. Her only option was a private treatment facility, which cost $40,000. Trinlie’s insurance company would only agree to reimburse the cost, leaving Trinlie scrambling to find the money upfront. She began the lengthy process of refinancing her house, but before she could come up with the money, it was too late. Zoë died of a drug overdose on August 6, 2014, just days after she turned 18.
To get into an abstinence-based treatment center, you need to go through detox first. But a detox center can be really hard to find.
Detoxification, or detox, is a period of abstinence during which your body rids itself of illicit substances. Usually lasting 3-5 days, detox is a pre-requisite to any abstinence-based treatment center. Unfortunately, it’s often harder to get into detox than treatment itself due to a lack of availability. The resulting “bottleneck” keeps many people desperate for help locked out of the treatment system altogether.
The extraordinary lengths that some people will go to circumvent a detox “bottleneck” are illustrative of just how little the current treatment model is able to meet demand. One of the more drastic measures that some drug users employ is to convince emergency room personnel that they are suicidal. Most free or affordable detox centers are located in county hospitals and the only way to bypass the waiting list is to walk into an emergency room and declare oneself suicidal. Unfortunately, emergency room personnel have come to recognize that many of these people are not actually willing to kill themselves, and so the “pretenders” are often turned away. The people who win the coveted fast-lane ticket to detox are the ones who put on the most convincing display of “crazy” or who actually inflict self-harm.
Also related to self-harm is the tragically common method of self-detox, or quitting drugs cold turkey when no detox center is available. Detoxing from a serious drug or alcohol addiction at home without medical supervision is agonizing and extremely dangerous, but for many who have been denied entry into a detox facility, it is seen as the only option.
Pastor James Sizemore of Radiant Church in Fayetteville, North Carolina, has helped several of his parishioners to self-detox. He recalls one example of a mother who showed up at church begging for help for her 23-year-old son, who was addicted to heroin. Her son had tried to get into the county detox center, but was repeatedly turned away because there are only eight beds available for the city’s 200,000 residents (If Fayetteville’s drug and alcohol addiction rates are on par with the rest of the United States at 8.6% that means eight detox beds for an estimated 17,000 people who need them). James spent five days at the family’s house helping the young man detox using over-the-counter medications to alleviate some symptoms, which include extreme pain, diarrhea, vomiting, uncontrolled blood pressure and itchiness all over the body.
“It was the most excruciating thing to witness,” says James. “I had to hold him back from running out of the house to get heroin because he was in agony. It took five days for him to get to a point where he could function again.”
Unfortunately, even those who risk the torture and danger of self-detox aren’t guaranteed access to treatment. With the exception of the young man, the majority of people who James helped self-detox were unable to get into a treatment center due to other barriers and eventually went back to using drugs.
“Going to treatment” is not as easy as we think.
The obstacles and catch-22s mentioned in this article are just a partial list of potential barriers that a person can encounter when seeking abstinence-based treatment (non-abstinence-based options such as opioid substitution therapy are available in some areas for some addictions, but that is a topic for another article). Not all the barriers listed above will prevent a person from enrolling in treatment all of the time. In fact, each treatment program has its own unique list of requirements and conditions. Some programs will take people with mental health issues, felony convictions, etc. Additionally, the Affordable Care Act is making strides towards increasing treatment access, particularly in states that have expanded Medicaid.
I want to make it clear that I am neither discouraging people from seeking treatment nor blaming treatment centers or staff for the numerous barriers that exist. Many treatment program staff work tirelessly to help people through recovery, and I understand how a facility, especially one that serves clients without resources or insurance, would struggle to accommodate people with special needs such as mental health or a criminal past. In fact, just as people who use drugs are often unfairly blamed for not getting into treatment, treatment centers are often unfairly blamed for not “fixing” a complex problem in a short time with few resources.
My intention is not to scapegoat, but to point out that instead of asking why people who use drugs don’t “just go to treatment,” we should be asking why treatment is so difficult to access in the first place. Why do governments struggle to come up with funds for recovery programs while offering generous grants and military equipment to fight the so-called War on Drugs? Why do treatment centers turn people away while jails will always find space for a drug user? Why do we refuse to adequately address mental illness and then condemn people for self-medicating? At the end of the day, if we really want people to seek treatment for drug addiction, then we need to fix the system and we need to fund it.
Tessie Castillo is the Advocacy and Communications Coordinator at the North Carolina Harm Reduction Coalition. She writes a regular column for The Huffington Post on overdose prevention, drugs, sex work, HIV/AIDS, law enforcement safety and health. She last wrote about sexism in the drug war.

