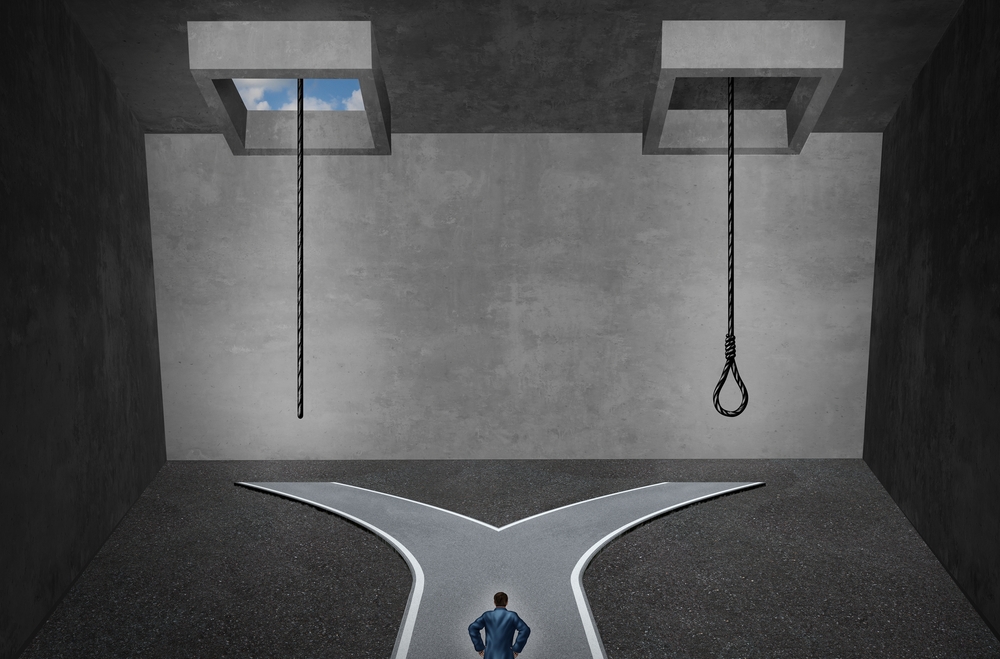
Addiction therapists have always confronted significant challenges, but providing treatment in the context of the current opioid epidemic has raised the stakes to new levels. Comorbidities that are extremely prevalent in addictions—trauma, physical pain and depression, to name a few—have their own correlations with suicidality. And the increasing percentage of treatment episodes in which opioids are the patient’s drug of choice—and the widespread easy availability of opioids—ups the ante for clinicians and suggests that greater vigilance around potential suicidality is required. We don’t have a good way to determine what percentage of overdose deaths involved an intentional suicidal component. Richard Kensinger is a clinical social worker whose expertise in the realm of patient suicide has been hard-earned, and his piece highlights the “grave responsibility” that clinicians have to evaluate client dangerousness by way of preventing avoidable self-harm…Richard Juman, PsyD
One of the most complex concerns and responsibilities for mental health and addiction clinicians is to discern and gauge the dangerousness that clients pose to themselves. I’ve spent over 40 years as a clinician dealing with clients who present with serious, recurrent, and persistent clinical disorders, a group that poses a great deal of suicide risk. Risk is high for self-harm in those suffering from schizophrenia, clinical depression, bipolar disorder, certain personality disorders, and in those who exhibit substance use syndromes. I’ve encountered clients who committed suicide, as these clients are much more a danger to themselves than to others. And I’ve counseled surviving significant others who are processing these violent endings. To the non-clinical person, they all seem so senseless and they are quite devastating.
I’ve also conducted a dozen “psychosocial autopsies” involving the active clients at a large mental health center, and one in a college setting. I’ve engaged in an extensive investigation of each death, referred to as a root-cause analysis of these “sentinel” events. And, I’ve engaged in critical stress-debriefing of clinicians and significant others.
These experiences taught me that even clinical teams can miss some of the clear and known risk factors. Even the most knowledgeable and experienced therapists may eventually lose a client to suicide. The devastation that we clinicians experience is intense when we lose clients in this manner. And significant others have many unanswered questions to ask once the shock and disbelief diminishes.
Dealing with actively suicidal clients before-and-after recovery, and based on these autopsies, I’ve also discovered what I refer to as the “suicidal trance.” I find this to be the threshold of no return when clients are no longer ambivalent about taking their own life. In addition to hopelessness, I see helplessness and worthlessness as additional risk factors. Once crossing this threshold, the client can even justify that they will not be missed, and that, in fact, they are doing others a favor.
My first encounter with a client suicide was “Tony,” a 28-year old single white male. He subsisted on disability due to his mental health condition—bipolar disorder with schizoaffective components. He was a longstanding patient in the mental health clinic, and I worked with him for over four years. For most of the time that I worked with him, he was reasonably stabilized on psychotropic medications, and he responded well to supportive psychotherapy. We established a strong therapeutic alliance, he was generally respectful, polite and cooperative, and he exhibited a great sense of humor. I liked him. He drove a Grand Prix automobile, which was his pride and joy. He was estranged from his family-of-origin, and lived at first with a woman who had a young son that was not his. She was quite marginal in her functioning. In addition to our individual psychotherapy, I also worked with them both in couples therapy.
In time, Tony relapsed into mania and I petitioned for his involuntary commitment. He returned to his pre-mania state after discharge, but eventually his girlfriend tired of him and abandoned and rejected him. He was initially despondent, but quickly found another woman to take him in who was more intact than Nancy. I resumed individual and collateral therapy and he quickly reconstituted. However, in time his new girlfriend also rejected him, leading to a renewal of his depression. As a result, I began to see him more often, but over a period of a few sessions he became more detached.
I was out washing my car on the weekend when I got the call from our crisis team: Tony had jumped from a railroad bridge and died almost instantly. Before I became his therapist he had attempted suicide in this manner and survived without any serious physical residuals. I was surprised and not. I attended Tony’s viewing; His two “exes” were there. I felt very sad, and believed that I had let him down. They comforted me by indicating that he was “lucky” to have had me as a therapist.
After the suicide, I consulted with a senior clinician and explored the loss at length. I realized that I had failed to respond adequately to his growing despondency. After this experience, ever-vigilant to increasing depression and withdrawal in my patients, I didn’t lose another client to suicide over a 20-year span.
Further on in my career, I was called in to perform a psychological autopsy following the suicide of “Michael,” a 15-year old who was attending a private Catholic school. The school provided an intimate environment for students, and the spiritual aspect was definitely an integral foundation underlying the student’s education.
He had been referred to our in-house student assistance program (SAP). All of the faculty members there were well-trained, and there were also two masters-level mental health clinicians. He was referred because of low-academic performance, and academics were highly valued there. So were athletics, and Michael was not involved in sports, so he felt inadequate around his peers. There was nothing else in his biopsychosocial presentation that was remarkable, and he was actually well-liked by his peers. I was called in for consultation after he hung himself. The SAP team was shocked and very distressed. I performed a Critical Incident Stress Debriefing and a psychosocial autopsy.
The autopsy revealed little about his motives. We discovered, however, that at least 14 of his peers knew about his plan, in regards to the date, day and method, and no one alerted the SAP team! In a span of three years, two more students killed themselves, and so did one faculty member, but none of those folks had been referred for counseling. Unfortunately, we are not yet very good at predicting behavior, including suicide.
In working with patients with addictive disorders, trying to determine death by suicide can be difficult. Obviously, we are in the middle of an epidemic of opioid overdoses. Often, these deaths are ruled as “accidental.” But are they? How many of these deaths are truly “accidental” as determined upon autopsy, and how many reflect clear suicidal intention?
Let’s look at three recent “celebrity” deaths: Amy Winehouse, Heath Ledger, and Philip Seymour Hoffman:
Amy Winehouse died at age 27 of a “voluntary and deliberate” intake of alcohol that exceeded five times the legal limit. Her death was not ruled a suicide.
Health Ledger died at age 28 due to “accidental” ingestion of the following agents: oxycodone, hydrocodone, Valium, Ativan, Xanax and doxylamine, used for insomnia. These are all controlled agents and potent CNS depressants that can lead to respiratory arrest. His death was not ruled a suicide.
Forty-six-year-old Phillip Seymour Hoffman died of an injection of heroin, cocaine, amphetamine, and benzodiazepines. His death was not ruled a suicide.
I did not treat any of these celebrities, and the information that I have presented is from public sources and coroner’s findings. But in thinking about their deaths, I find myself wondering if the signs of the “suicidal trance” were discernible, if they had crossed the point in which the longing to live was no longer powerful enough to ensure their safety.
Can we prevent some of these deaths? The major risk factors of suicide are well known: male gender, clinical depression, alcohol, access to weapons, hopelessness, helplessness, and worthlessness. Despite our clinical knowledge, we cannot predict with high accuracy which of our active clients will attempt suicide. The abuse of powerful psychoactive substances is widely recognized as very destructive and leads to premature morbidity and mortality. In particular, the potent CNS depressants are more lethal than the psychoactive stimulants, causing many users to die of respiratory arrest. In regards to substance use disorders, multiple relapses are not unusual, and with each relapse the risk of overdose death increases.
During my clinical career I’ve conducted a number of psychosocial autopsies and root-cause analyses of active client deaths. Most of these deaths were ruled suicides by the local coroner in our region. The clinicians who I consulted felt a deep responsibility for failing to protect their clients. In many of the cases, I concluded that the clinicians missed vital and key information. There were often clear indications of suicidality that were not given the attention that they might have been.
So what are clinicians to do when working with persons showing dangerousness? Clinicians are vested with these simultaneous duties regarding dangerousness: warn, protect, predict and prevent. The research is clear that we are poor in predicting dangerousness, despite our clinical expertise, and that we don’t have to be absolutely convinced in terms of our prediction. Therefore, it is imperative when working with these clients, to conduct a biopsychosocial history that includes the known risk factors for suicide and to do this on a periodic basis until the crisis has resolved. We need to assess based on what we know about the client, and based on what we “should know.”
In other words, we follow the best-known practices. Gaining critical collateral information about my clients has always been an informed practice of mine. Of course, I do this with client consent, which can be waived in times of a crisis. From there, I make a determination about the appropriate level of care, with the patient’s safety foremost in my mind. We certainly can use the involuntary commitment as I have in some situations. Here in Pennsylvania, we can petition the court to have someone evaluated by a medical professional. This evaluator can then determine the necessity of a brief hospitalization. In this state, we can also commit a person to non-inpatient levels of care. However, this situation can be more complicated when clients are actively under the influence of mood-altering psychoactive substances.
My purpose here is not to disparage clinicians. I am one, and I am certain that we save many more lives than we lose. My intent is to illustrate the grave responsibility we encounter in dealing with client dangerousness, and to spark further dialogue with my peers. I know we can all enhance our clinical competencies by such means.
I hope that these ideas can be further digested and discussed in this particular forum. Although we cannot prevent all deaths of active clients, we can diminish the number of lives taken via suicide. For two years I co-conducted a support group for those who lost someone to suicide. One of the prominent issues in this group was to understand the “why did they do it?” question. Although I could only provide them with some of the answers, and it did not diminish the devastation felt, it began to make more sense to them.
Richard Kensinger, CSW, is an adjunct faculty member in Psychology and Community Counseling @ Mount Alouysius College located in Cresson, Pennsylvania, where he teaches at the undergraduate and graduate levels. He has been a practicing clinician in healthcare and behavioral healthcare for 44 years, and conducts clinical training and consultation via his private practice, The Center for Ethics in Human Services. He can be reached at rkensinger@mtaloy.edu
