Quitting smoking is hard, as any nicotine addict will tell you. So hard, in fact, that a popular 2011 article in The Fix reported that nicotine is the third most addictive substance, behind heroin and crack cocaine, in terms of how hard it is to kick.
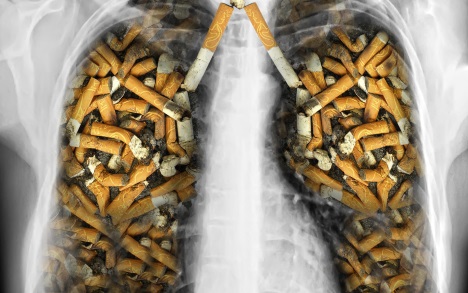
The statistics surrounding nicotine are, indeed, grim. There are 50 million nicotine addicts in the US, and one in five deaths results from smoking. Not only is smoking—and related activities, like chewing tobacco—addictive because tobacco contains nicotine, but tobacco also contains more than 19 carcinogens as well as more than 4,000 other chemicals. According the CDC, smoking is the leading preventable cause of death in the United States. Smokers are more likely than nonsmokers to develop heart disease, stroke, and lung cancer. In fact, smoking can cause cancer almost anywhere in the body.
Many smokers know all this, yet continue to smoke. For smoker John, whose name has been changed for this piece, quitting is anything but a simple cost-benefit analysis.
“I think I started [at 13 years old] because the kids I was hanging around with smoked,” he says. While that sublime sense of “calmness” he used to get is long gone, he understands that he needs to smoke. “I don’t think I recognize the high, but I get it physically.”
Biology of nicotine addiction
Nicotine is a compound found in the nightshade family of plants (Solanaceae) and a stimulant drug. It is a nicotinic acetylcholine receptor agonist, which means it can bind as well as acetylcholine to the acetylcholine receptor.
Acetylcholine is the oldest neurotransmitter and acts throughout the body and brain on the autonomic nervous system. The autonomic nervous system is essentially the hardware of our bodies, running unbeknownst to us in the background and maintaining essential bodily functions, controlling our GI system, and stimulating the fight-or-flight response when needed. It’s possible that the difficulty in quitting smoking is directly related to that fact that acetylcholine’s effect on our bodies is so varied and ubiquitous.
There are two main types of acetylcholine receptors: the nicotinic acetylcholine receptor (nAChR), which is so named so because it is responsive to nicotine; and the muscarinic acetylcholine receptor (mAChR), which responds particularly well to muscarine. There are many receptor sub-types of the nAChR, but nicotine has a high affinity for the one in which the β2 subunit is coupled with α4 or another subunit. Chronic exposure to nicotine “up-regulates” these specific receptors, which enhances craving and worsens withdrawal in smokers.
The effects of ingesting nicotine are widespread. About 20 seconds after smoking a cigarette, nicotine binds to the nAChRs in the brain and increases the level of several neurotransmitters, including dopamine, norepinephrine, and serotonin. Because nicotine activates the autonomous nervous system, prompting the release of adrenaline, this causes an increase in heart rate, blood pressure, and respiration, among other things.
In fact, nicotine can act as both—or alternately—a stimulant and a relaxant. Increased acetylcholine improves concentration and memory; more norepinephrine enhances alertness and arousal. Increased beta-endorphin reduces pain and anxiety. More dopamine works to give pleasure and increase the sensitivity of the brain’s reward system to nicotine.
In moderation, nicotine’s effects are generally good. In small, therapeutic doses—an entire area of scientific study—nicotine can be used to promote well-being. However, from the standpoint of nicotine addiction, one cigarette is too many for some people.
Withdrawal sucks
Craving is a “physical tic,” John says. He gets irritable, anxious, and automatically goes for a smoke. “It’s hard to say what’s a physical urge and what’s just going about the routine. I don’t think about it, I do it.”
Withdrawal is what keeps nicotine users addicted, whether they are conscious of this process or not. The symptoms of nicotine withdrawal usually appear approximately two hours after the last dose. Common symptoms include an intense craving for nicotine, anxiety, depression, drowsiness, bad dreams or trouble sleeping, feeling restless or frustrated, headaches, increase in appetite, weight gain, and difficulty concentrating.
“I think about quitting, but I talk myself out of it,” John says. “I make up one reason or another and say, ‘I’m not prepared to go through this.’ I’m not thinking about how it’s going to feel to not have a cigarette for the next hour, I’m thinking about, I don’t want to go through the next month.” Cravings last for a long time, he says. He once quit for two years, but the cravings never went away completely. “Two years later, I had a craving and a cigarette and then three days later, I was smoking a pack a day again.”
Addicted from the first cigarette?
In the 1960s and 1970s, researchers started exploring the idea of tobacco addiction, but it wasn’t until the 1980s that the mechanism behind this addiction—that nicotine acted on a well-studied receptor and improved mood and memory—began to be elucidated. The 1990s saw the first drugs to treat the withdrawal associated with nicotine abuse.
In 2008, Dr. Joseph DiFranza, professor of family medicine and community health at the University of Massachusetts Medical School, wrote a piece for Scientific American magazine about the effects of just one cigarette. His novel theory at the time says that one cigarette is all it takes to become addicted—by definition, this means experience withdrawal symptoms.
“It is now clear that the brain reacts rapidly to the first exposure to nicotine in ways that alter its structure and function,” DiFranza says. “We do not know exactly what these alterations are doing to the brain to cause addiction, but our best hypothesis is that the brain reacts quickly to counter the effects of nicotine. As a result of these countermeasures, the brain is no longer in balance when nicotine is absent. Anytime the brain has gone too long without nicotine it generates a craving for the drug.”
Laura Bierut disagrees. “I do not believe that we become addicted from the first cigarette,” she says. “There is very strong data that some individuals smoke lightly for long periods of time.” Bierut, who is a professor of psychiatry at Washington University School of Medicine and who has led the Collaborative Genetic Study of Nicotine Dependence (COGEND) study for nine years, believes that our increasing knowledge of genetic susceptibility to becoming addicted to nicotine will lend more nuance to the question, Why do some people become addicted?
Genetics plays a role in addiction, as we know from twin studies that show that in general, addiction is half genes, half environment. In nicotine addiction, receptor subtypes are important to understanding the severity. In other words, the nicotinic receptors of the person who becomes addicted are not the same as those of the person who does not. Variants within a cluster of nicotinic receptors on chromosome 8, CHRNB3-A6, have been associated with cigarette consumption in several genome-wide association studies (GWAS)—specifically that a variation in the cholinergic nicotinic receptor subunit α5 (CHRNA5) increases the risk for developing a dependence on nicotine. Nicotine addiction has been found to frequently co-occur with bipolar disorder and alcoholism, adding another layer of complexity to the problem. Finally, there are both genetic- and environmentally-influenced differences between individuals and ethnic groups in how nicotine is metabolized.
Treatment
There are a variety of treatment modalities out there, and it depends on a variety of factors as to which one will work best for an individual.
- Smoking cessation aids
These can come in many different forms, but they can be generally categorized as nicotine replacement therapy—patch, gum, lozenges, and others—and medications to help with cravings and withdrawal—bupropion (Wellbutrin) and varenicline (Chantix) are two.
The bad news is that today’s smoking cessation treatments have modest long-term success rates. In fact, research has shown that less than 25% of smokers remain abstinent a year after treatment. Scientists are looking into ways to improve upon this disheartening statistic. In a recent study published in June in the American Journal of Psychiatry, researchers found that combining two smoking cessation therapies—adding bupropion to varenicline—is more effective than using just one method, for smokers who weren’t initially helped by the nicotine patch.
“The combined treatment had a much greater effect on male smokers and those highly dependent on nicotine, while no significant difference was seen in female smokers or those with lower levels of nicotine dependence,” says Jed Rose, director of the Center for Smoking Cessation at Duke University and the study’s lead author. “One possible explanation is that male smokers have been found to have a deficit in brain receptors for dopamine, which is one of the key chemicals involved in addiction. Bupropion works in part by raising the level of dopamine signaling in the brain, and so male smokers might have derived a greater benefit when bupropion was added to varenicline treatment.”
Another recent study, published in JAMA in July, found that combining varenicline with nicotine replacement therapy was more effective than varenicline alone for abstinence at six months. However, the study showed that in the combination treatment group, there was more nausea, sleep disturbances, skin reactions, constipation, and depression; the varenicline-only group experienced more abnormal dreams and headaches.
- Nicotine vaccine
While there is hype surrounding a vaccine for addiction, especially for cocaine and now, nicotine, NicVAX has not yet lived up to it. As a conjugate vaccine—a nicotine-based molecule linked to an antibody to nicotine—NicVAX works by binding to nicotine, effectively quarantining it in the blood, and thereby preventing it from binding to nicotinic receptors in the brain.
While early trials showed promise, two Phase III trials from 2011 failed—the vaccine worked no better than a placebo. A proof-of-concept study published in the American Journal of Psychiatry in 2013 showed that indeed, immunization led to a 12.5% reduction in nicotine binding to a specific nicotinic receptor as well as a 40% reduction in cigarette use and a significant reduction in craving for cigarettes. However, the study’s clinical validity was compromised by its small subject size and lack of control group, among other factors.
In a very recent study published in Addiction in August, scientists concluded that NicVAX “does not appear to improve the chances of stopping smoking when given in addition to varenicline and behavioral support.”
- Treatment programs
Treatment programs, like the 12-step-based Nicotine Anonymous or inpatient courses, might work for some. The eight-day residential treatment program at the Mayo Clinic Nicotine Dependence Center in Minnesota “provides the most intensive treatment option available for stopping smoking,” according to its web site. More than 1,300 people have been treated since the program began in 1992. Two other inpatient programs are at St. Helena’s Center for Health in Deer Park, California and Hazelden’s Next Step program.
Genetic testing
Why are some smokers more addicted than others? “Addiction depends on both a genetic predisposition and experience with nicotine,” Rose says. “Similarly, both genetic factors and environment influence the ability to successfully quit smoking. Situations eliciting stress or negative mood are the main precipitants of relapse among those trying to maintain abstinence.”
Several studies show that genotyping patients before prescribing them cessation aids will work better, in other words, have better quitting outcomes. In one study, published in 2007 in the journal Nicotine & Tobacco Research, scientists conducted a randomized, double-blinded, placebo-controlled trial examining genetic influences on treatment response to sustained-release bupropion. They found that a specific genotype, or mutation, of the dopamine D2 receptor might influence treatment response to bupropion.
Not only do genetic differences influence a person becoming addicted, but there are “robust genetic influences likely for individual differences in abilities to quit,” write the authors of an article published online in 2012 in the journal Molecular Psychiatry. In this study, co-authored by Rose at Duke, the scientists were able to identify mutations that could predict the success of quitting smoking, but also that these same genetic factors influence the rate of becoming addicted (to anything) during adolescence.
Says DiFranza, “Some people are more addicted than others, some have better support systems and coping skills, and people certainly differ in how they experience nicotine withdrawal.”
Indeed, the process of quitting—or, trying to quit—is an ongoing one for John. His incentive to quit for those two years was a coughing fit behind the wheel of his car. He was fed up, but also, “I wasn’t going to let myself fail.” At the time, he was working in an office where everyone knew he was quitting. He picked up running, and that seemed to help, too. “Environment has a lot to do with it,” he says.
Jeaneane Swanson is a regular contributor to The Fix. She last wrote about the unhappy side effects of anti-depressants, erasing your traumas and alcoholism and genetics.
