The steady increase in overdose deaths in the United States in recent years has reached what advocates and the media call “epidemic” proportions. Drug overdose is now the leading cause of accidental death for adults. It’s become such a problem that President Obama appointed a National Heroin Task Force, and it’s become a hot topic on the presidential campaign trail—Hillary Clinton has a specific plan laid out in her platform.
People, mostly people of color or poor white people in cities or rural areas, have been dying by overdose from heroin and other drugs for decades. They’ve traditionally been met with prison time and criminal records, which rob them of opportunities and reinforce their reasons for using drugs. Many of us remember the “Just Say No” and “This is Your Brain on Drugs” campaigns of the 1980s, their spectacular failures, and how they fed into the fear and frenzy of the emerging “crack epidemic” and the subsequent “tough on crime” stance politicians took in the 1990s.
The resources which are being doled out by federal and state agencies won’t make it to the areas which need them most.
Now, heroin has made its way into suburbia. Actually, let’s take a step back. Heroin has been in suburbia. I started using in 2004, at the age of 25, and it had already spread to every pocket of metro Atlanta, a region where heroin has not traditionally been popular. Now, more people are dying, including young, white, middle-class kids in the suburbs. Their parents wield greater influence. Their faces stir up an emotional response denied to other victims of this overdose crisis. And now that these communities are feeling the same pain that poor inner city and rural neighborhoods have suffered for decades, we see this calls for a gentler response, for prioritizing treatment over incarceration.
In Alpharetta, Georgia, an affluent suburb of Atlanta, Director of Public Safety Gary George recently offered concerned parents this advice:
Call the police. We’ll come out to your house, take the drug dogs and search your house. ‘Here, dad. Here’s the drugs. Here’s the marijuana, here’s the heroin, whatever it may be.’ Now if you say, ‘I want him to go to jail,’ we’re probably going to argue with you about that. Jail’s not the right thing to do here.
This might be how things work in mostly-white Alpharetta, but anyone with a history of police encounters, especially in communities of color, probably isn’t buying what George is selling. His attitude further demonstrates the dual-nature of the U.S. justice system, where five times as many whites are using drugs, but black people are sent to prison for drug offenses at 10 times a higher rate.

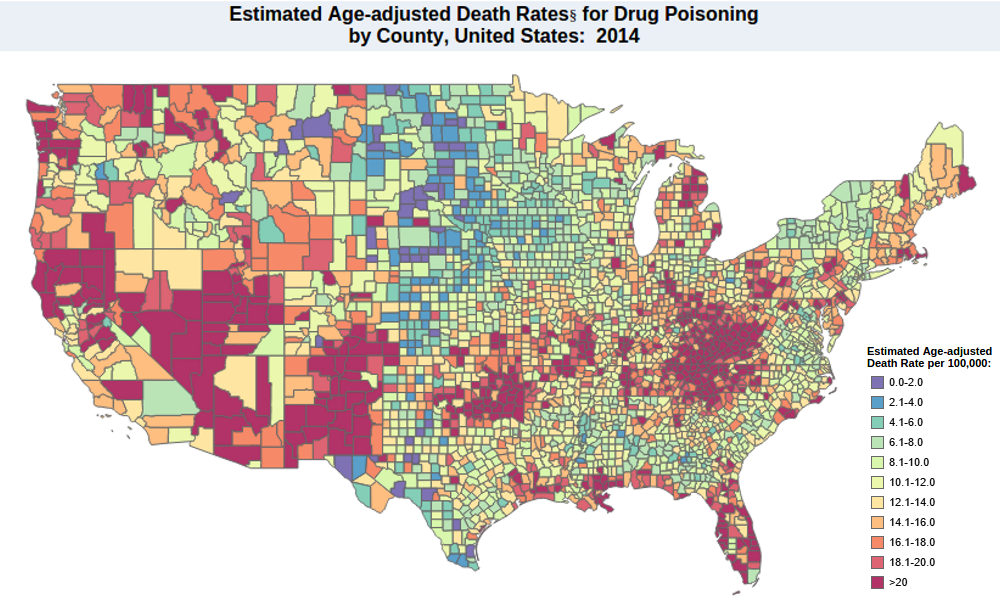
U.S. overdose death rates for 2014 by county (Source: CDC/NCHS, 2014)
This isn’t to say that white suburban kids aren’t suffering. Many are shuffled from one high-priced rehab to the next, their college funds drained while their parents desperately search for something that works. It’s a tragedy and it’s painful to watch. To echo statements made by politicians who have conveniently ignored the problem for years, this is an issue that transcends every demographic. Unfortunately, this newfound compassion, and the resources which accompany it, do not.
The dominant cultural narrative of the past few years is that addiction and overdoses are disproportionately impacting young, white, middle-class suburbia. But the most recent CDC statistics from 2014 paint a different picture. While substance use, especially heroin, has increased in those areas, overdose deaths are, by far, hitting much harder in other places.

Overdose rates by age group, 2014. Source: CDC/NCHS
Every age group between ages 25 to 64 died by overdose at substantially higher numbers than the 15 to 24 age group. Looking at the map of which counties are seeing the highest overdose rates, a clear picture emerges. We see numbers of >20 per 100,000 people dying from overdoses in almost every corner of poor, rural Appalachia. Native Americans, who die from overdose at twice the national average, are being hit in Minnesota, Oklahoma, and New Mexico. And rural areas of Utah, Nevada, Arizona, Northern California, Montana, and Washington are well above the national average. Mostly-rural states like West Virginia, New Mexico, Kentucky, Nevada, and Utah led the nation in overdose death rates in 2014.
Death rates for whites doubled between 2002-2014, but they’ve also increased across all demographics. And, when combined, people of color—black, Hispanic, Native American—still die at a higher rate, even though they use drugs in lower numbers than whites.
This is a problem which impacts every group in the United States, but resources aren’t being evenly distributed. Harm reduction and drug policy reform advocates have been calling for a broader focus on treatment and public health services over incarceration and punishment for decades. We’ve made headway in passing laws which broaden access to naloxone—trade name Narcan, the medication which reverses most opiate overdoses. But racial and class disparities in who’s being punished persist, and politicians continue to reinforce false stereotypes that people of color are providing most of the drugs to the growing white consumer base.
Treatment is readily available in suburban communities, while effective medication-assisted treatment (MAT) with medications like Suboxone is out of reach for most rural and urban communities. Methadone clinics are sometimes impossible to locate. (Methadone is the most effective long-term treatment for reducing mortality, relapse, property crimes, recidivism, and disease transmission.) In the entire state of West Virginia, which has the highest death rate, there are nine clinics. East Tennessee, an area which has been hit especially hard, has only three clinics—two of them in Knoxville. (This, despite efforts by advocates to open more clinics in the region.) It’s not uncommon for patients to make daily trips across the Smoky Mountains to visit clinics around Asheville, North Carolina—trips which can take over an hour each way. Methadone treatment has been specifically targeted to urban communities, where it is affordable and covered by Medicaid in some cases, but also carries a heavy stigma and much tighter regulations.

Overdose rates in rural America have overtaken metropolitan areas. (Source: NY Times)
Access to Suboxone remains limited or virtually inaccessible to poor, urban and rural opioid users looking for help. A 2015 Huffington Post feature brought attention to the overdose crisis and lack of access to Suboxone in Kentucky, where people in traditional 12-step rehabs and drug courts were denied MAT and died in droves after leaving the programs. Today, there are long waiting lists to see Suboxone doctors and access is limited to those who are able to afford the high costs.
The number of patients a doctor can treat with Suboxone is limited by the federal DATA 2000 Act to 30 in the first year, and up to 100 patients after that. This leaves little incentive for psychiatrists or addiction experts to jump through hoops to treat substance users who are already stigmatized. Many times, it’s family practice doctors with little experience in addiction treatment who pick up the slack. Doctor visits are usually cash-only, and even with insurance, the cost of Suboxone can run well into the hundreds of dollars for a month’s supply.
A report by the president’s Heroin Task Force calls for a doubling of the number of Suboxone doctors, expanded access to MAT, incorporating MAT into the criminal justice system, expanded access to naloxone (which we haven’t even touched on here), and steps to “mitigate the dangers of intravenous drug use” (a high risk factor in HIV and hepatitis C transmission, which we also haven’t touched here). Many states have formed their own task forces to address the problem, but states like Tennessee are moving backward by restricting access to Suboxone. Opiate users in the state commonly complain of being unable to find doctors, and when they do, they report problems getting prescriptions filled.
There’s no doubt that changes to U.S. drug policy and mass incarceration are coming, but they aren’t coming fast enough. A more pressing issue, however, is that the resources which are being doled out by federal and state agencies won’t make it to the areas which need them most. It’s a promising sign that Americans want a more compassionate, public health approach to substance use, but we need to be careful that we don’t repeat the mistakes of the past and create more barriers for populations who have been suffering and searching for solutions for decades.
Jeremy Galloway is a co-founder and Education & Outreach Coordinator for Georgia Overdose Prevention, Overdose Prevention Coordinator at Families for Sensible Drug Policy, a certified peer recovery specialist, public speaker, and a certified SMART Recovery meeting facilitator in the North Georgia mountains.
