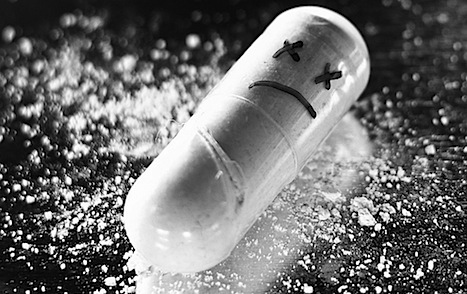
In 1804, Frederich Serturner experimented with opium and created something new—morphine—named after the Greek god of sleep and dreams, Morpheus. More than 200 years later, at least 8 million Americans fall asleep at night under the influence of an opioid. Every morning, 40 of them don’t wake up.
As described in a previous article on this subject, the United States is in the grip of a prescription opioid disaster: with 2 million people addicted, drug overdose is now, for the first time, responsible for more deaths than car accidents, and prescribed opioids are responsible for most of the fatalities. What can be done to control this epidemic?
In reality, there are two separate problems. First, what should be done for the millions already hooked on Oxycontin, Vicodin and other opioids? How can we prevent so many of them from becoming part of next year’s statistics? Second, what can we do to prevent the next 2 million, people who are showing up in physicians’ offices now, seeking treatment for their chronic pain, those looking for relief but putting themselves at risk for addiction?
“It’s hard for physicians to say ‘no’ when patients demand opioids for pain because both patients and physicians have come to believe that opioids offer a solution.”
Members of both groups have at least one thing in common: they live in a country that assumes, whatever ails us, that there will be a quick, complete and external fix for it. According to Jane C. Ballantyne, MD, FRCA, Professor of Education and Research in the Department of Anesthesiology and Pain Medicine at the University of Washington, a pre-eminent authority in pain management, “We live in a culture in which the expectation is that we can ‘fix’ everything.” Unfortunately, because of now-suspect research, overzealous marketing by the pharmaceutical industry and a campaign that encouraged doctors to stop being “opioidophobic” about pain, Dr. Ballantyne notes that “it’s hard for physicians to say ‘no’ when patients demand opioids for pain because both patients and physicians have come to believe that opioids offer a solution.”
Physicians frequently prescribe opioids for use in the treatment of acute pain, in some cases without exploring the patient’s substance use history or assessing for the risk of addiction- a problem in and of itself. But with respect to longer term use, it really seems to require a master’s touch in order to use opioids safely and effectively. For example, Mark Willenbring, MD, former Director of the Treatment and Recovery Research Division at NIAAA/NIH Founder and CEO of Alltyr: Addiction Treatment for the 21st Century, believes that opioids can be “very helpful in restoring function in chronic pain”, but bemoans the fact that “there is no consensus about who should receive how much opioid and for how long” and notes that doctors need “much better education in pain management and opioids.”
While experts may disagree as to whether there should be any role for opioids in managing chronic pain, they agree that the long term use of opioids is not the answer. Put simply, they just don’t do a good job of managing pain in the long run. According to Anna Lembke, MD, at Stanford University Medical Center, “it’s important to realize that opioids are not actually very effective for chronic pain, and can in some instances even make pain worse by causing a condition called ‘opioid-induced hyperalgesia’.”
So, unfortunately, there really is no single, simple “magic bullet” solution to chronic pain. Chronic pain is a long slog of a burden that needs to be met full-on by an actively engaged, motivated, psychologically resilient, hard-working patient if quality of life is to be maintained.Seen in this light, out of all the options available for chronic pain, opioids are in a class all by themselves in that they not only often fail to work, they cause addiction and death. According to Dr. Ballantyne, “We shouldn’t be using opioids at all for chronic pain, except in very unusual circumstances. Every medication that is used for pain tends lose its charm after a certain period of time.” Unfortunately, she notes, when the opioids stop working the patient is “unable to stop because of dependence and bad side effects.” Better never to start.
The Two Million
But it’s too late never to start for the two million Americans who are already living with the physical and psychological agonies that result from the multiple stressors of pain, opioid addiction and fear of overdose, not to mention the various severe side effects of chronic opioid use: sedation, tolerance, constipation, sexual dysfunction, etc. It’s a deep, dark hole to climb out of, but it can be done. According to Andrew Tatarsky, Ph.D. the Director of the Center for Optimal Living, an addiction treatment program in Manhattan, many patients come to treatment with a vast ambivalence towards their drug and their physician. “They love and crave their drug, the euphoria and the relief,” Tatarsky says. “But they also hate it because they know they’re both physically and psychologically addicted to a potentially dangerous medication, and suffering in a variety of ways. And they express a similar mix of emotions toward their physician, sometimes complaining that they weren’t properly advised about the risks, while at the same time experiencing a profound relief and gratitude every time they get a refill.”
Addiction treatment is a core ingredient in the recipe for working with people dependent on opioids for pain. According to Andrew Kolodny, MD, the Chief of Psychiatry at Maimonides Hospital in Brooklyn, “we have to make sure that patients addicted to opioids have access to effective addiction treatment. If we just close pill mills and make doctor shopping more difficult, without expanding access to treatment, people who are opioid addicted will turn to the black market for pills or heroin and overdose rates will remain high.”
The first step is getting patients who are addicted to acknowledge the addiction—that’s a huge part of the biopsychosocial trajectory towards recovery. Once that challenge is met, effectively managing the addiction is a goal that can be accomplished in several ways. Although nobody that I spoke with endorsed the idea of rapid detox fromopioids, many patients who are seeking treatment are admitted to inpatient detox, usually followed by a rehabilitation program. Others opt for Medication Assisted Therapy with a “partial opioid agonist” such as buprenorphine or methadone, which mimic some of the effects of traditional opioids but are less addicting. Dr. Lembke points out that “for people addicted to prescribed opioids, for whom abstinence has not worked, opioid substitution therapies such as methadone and buprenorphine are effective”.
Dr. Ballantyne notes that “these medications will also treat the pain, so you’re managing the addiction as well as the pain”. Adds Dr. Willenbring, “if everyopioid addict had access easily and cheaply to buprenorophine and methadone it would sharply reduce overdose deaths”. He also recommends “distributing naloxone injection kits to users/friends/families, which has been proven to reduce deaths.” Buprenorphine and methadone can be used to taper patients slowly from opioids to other forms of treatment for pain or used long term as maintenance therapy.
Experts are careful to point out that addiction is best treated in a comprehensive way. According to Susan Foster, V.P. and Director of Policy of Policy Research and Analysis at the National Center on Addiction and Substance Abuse at Columbia University (CASAColumbia), “a multi-pronged approach to addiction treatment that includes a combination of pharmaceutical and psychosocial therapies typically yields the best results.
How to prevent the next two million opioid addictions
What is the best approach for new patients? How can we prevent the next two million opioid addictions and the next 15,000 deaths? Only by changing the way we deal with addiction and chronic pain.
The solution must include, as an integral element, that prescribers develop a greater awareness of addiction. Frequently, little or no attention is given to a new patient’s historical relationship to alcohol and other drugs. Giving a prescription for Oxycontin or Vicodin to a patient without fully exploring past and current substance use is counterintuitive- but it happens all the time. “All physicians should routinely screen patients for risky substance use and addiction as an essential component of evidence-based medicine. This is particularly true in patients with pain or other conditions which may require controlled prescription medications”, notes Jayaram Srinivasan, MD, MPH, CPH, Senior Medical Advisor at CASAColumbia.
Experts agree that a “multimodal” approach to pain management is best. Since there is no “magic bullet” for chronic pain that will eliminate pain long term without causing side effects (or death), the best approach is to have a quiver full of arrows in the battle against pain. And the conversation that happens in the early stages is critical, says Norman Wetterau, MD, FAAFP, FASAM, President of the New York Society of Addiction Medicine. The language that is used to discuss these issues is critical, especially when patients walk in the physician’s office expecting that an opioid will be prescribed: “Rather than saying ‘I cannot give you opioids,’ you can say, ‘I have something better for your pain.'” And again, the best approach is often multidimensional.
According to Dr. Ballantyne, “there are a variety of alternative approaches that are ultimately more effective including psychological treatments, acupuncture, yoga, Tai Chi, tricyclic antidepressants and anticonvulsants.” Others find great relief through chiropractic treatments, meditation or relaxation training. And there are many non-addicting options available from a prescription pad. According to Dr. Srinivasan, “Effective non-opioid pharmacological treatment of pain may include numerous options such as aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), selective NSAIDs, anticonvulsants, tricyclics, serotonin-norepinephrine reuptake inhibitors (SNRIs), antispasmodics, topical analgesic agents, and others.” But Dr. Ballantyne reminds us that the “the single most important approach focuses on the psychological aspects of pain because the patient needs to be engaged, activated and motivated in order to achieve the best outcomes”. Again, chronic pain is an ongoing challenge, and only those who personally engage will get the best results. Those who passively expect their doctors to relieve their pain wind up in trouble.
Dr. Kolodny is confident that the medical community will be able to turn things around. In his role of President of Physicians for Responsible Opioid Prescribing (PROP), Dr. Kolodny devotes much of his time to making sure that physicians have the tools they need to weigh the pros and cons of opioid prescribing: “Doctors who realize thatopioids are dangerous and addictive, and that they don’t seem to work well for most people with chronic pain, will prescribe more cautiously.”
Note to Primary Care and Family Practice Physicians: On February 9, 2013, Dr. Kolodny and others will be speaking at a free lunch for MDs at the Yale Club, sponsored by The Fix, CASAColumbia and PROP. To RSVP to this discussion of physicians prescribing opioids, RSVP to melanie@thefix.com.
