The DSM V—the next edition of psychiatry’s diagnostic bible—will redefine addiction in ways likely to have long-lasting, real-world consequences. As I explored in my column last week, psychiatrists are eliminating the seriously problematic terms “Substance Abuse” and “Substance Dependence” and placing all related conditions into a single new category: “Substance Use and Addictive Disorders.”
I don’t foresee any negative results from dropping those two misguided terms. But what does concern me is the fact that rather than still having two separate and distinct conditions—one, a short-term, self-limiting disorder and the other a condition likely to be chronic and relapsing—there will now be only one way to have a drug problem. The gradations of the condition will likely be delineated as “mild,” “moderate” or “severe” substance use disorder. While the word “addictive” will appear in the heading that labels the overall category, it will not figure in the diagnoses themselves. For example, you could have mild, moderate or severe opioid dependence disorder or gambling disorder. (So far, gambling is the only behavioral addiction to make the DSM cut.)
But this elision of the problems formerly known as abuse and dependence will, I fear, cause major problems for many people, especially teenagers and young adults. What it means, in a worst-case scenario, is that every college binge drinker will be at risk for being labeled an alcoholic and every high school stoner, an addict. There are some scientific arguments favoring the proposed change. However, just as there was a clear case to be made for labeling addiction as “dependence” during the previous revision of the DSM ten years ago, these reasons similarly fail to take into account critical clinical and cultural realities.
The scientific rationale for creating a single substance use disorder is that the “invisible line” that distinguishes a really bad boozer who can regain control over his consumption and an alcoholic who cannot remains invisible.
Indeed, research shows that some people who meet the full criteria for alcoholism or addiction can return to controlled use—though this proportion decreases as severity of the problem increases. The data also shows that a large proportion of people who would currently be diagnosed as “substance dependent” recover without any type of treatment or self-help involvement at all.
In short, no one can predict which college drunk will go on to skid row—and which one will become President.
Because it’s so hard to tell where heavy use ends and addiction begins, the writers of the new DSM—want to place substance use disorders on a continuum, explicitly recognizing that we can’t currently distinguish between “addiction,” which is chronic, and “substance misuse,” which is not. And that’s a fair reflection of the scientific reality.
The “invisible line” that distinguishes a really bad boozer who can regain control over his consumption and an alcoholic who cannot remains invisible. No one can predict which college drunk will go on to skid row—and which one will become President.
The problem, of course, is that those ideas will be set free into a world in which the National Institute on Drug Abuse, the American Society of Addiction Medicine and the millions of members of 12-step programs define addiction as a “chronic, relapsing disease.”
All of these groups and, most importantly, the addiction treatment industry, tend to see everyone who takes a lot of drugs or drinks heavily at any point in time as having that disease. Some even diagnose any use of illegal drugs at all as addiction. This, not coincidentally, is in the economic interest of a quickly mushrooming rehab industry. In fact, in the ’80s, major chains of rehabs and psychiatric hospitals had to pay out big settlements in lawsuits over admissions of people who did not have the diagnoses the programs claimed (some were children kidnapped and held till their insurance ran out).
Even now, however, a great deal of treatment energy and time is currently aimed at trying to get people in recovery to admit that they have “the disease of addiction” and to label themselves as “addicts” or “alcoholics” in therapy groups. Counselors and other staff press clients to confess to a greater and greater problem severity, due to the pervasive suspicion that most people with addiction lie about how much they use. (This continues to be done in the face of research showing that doing so does not benefit recovery—if anything, “confronting denial” is linked with more relapse, not less.)
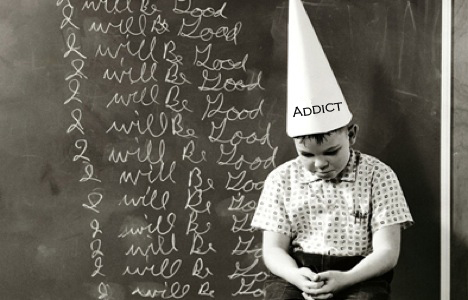
This push to adopt an addict identity happens even in adolescent treatment— despite the fact that most teens in treatment do not meet criteria for being addicted (some don’t even meet criteria for drug abuse!). Indeed, the vast majority are, not surprisingly, nondaily binge users of booze and pot. Nonetheless, at ever-younger ages, these kids are being pressured to view themselves primarily as addicts and alcoholics and to admit to having a chronic, lifelong illness with a 90% chance of relapse. Very little research has been done on the effects of this “treatment”—but given what we know about the fluidity of adolescent identity, it certainly has the potential to do significant harm.
For one, it can be a self-fulfilling prophecy—and I’ve spoken with quite a few people who have gone into adolescent treatment as marijuana users and emerged mis-using cocaine or prescription drugs, in part because they felt that they were “already addicts anyway.” Second, since research cannot predict which teens will outgrow their problems and which will have a chronic course, does it really make sense to have them all embrace a stigmatized identity centered around a disease?
By suggesting that every person who drinks too much or goes throug a period of frequent marijuana smoking is in the early stages of addiction, DSM V will help create an addiction epidemic. Without the category formerly known as “substance abuse” as a way to signal that the problem appears likely to be short-term, the presumption will be that “mild” substance use disorder is just the first step toward “severe.” This will only reinforce the already-troubling way that adolescent treatment centers label their patients.
It will also prop up the idea that abstinence is the only appropriate goal for treatment—even though a great deal of research supports treatments that do not require abstinence. Consequently, the new definition could undermine treatment aimed at moderation goals. And ironically, that’s often the only type of treatment that can reach people on the milder end of the spectrum. But if you see all substance use disorder as inevitably leading to addiction, you’re unlikely to see moderation goals as acceptable.
When I interviewed Dr. Allen Frances, professor emeritus at Duke University and Chair of the DSM IV Task Force—and a critic of the DSM V—for TIME.com [LINK], he shared my concerns. “I think the two terms have different meanings and different prognoses,” he said.
“Although there are people at the boundaries between the two, they shouldn’t be conflated. Most people with abuse don’t go on to become dependent. The overall category will be addiction and people who have a couple of DUIs in college are going to get a diagnosis of addiction,” Frances added.
NIDA Director Dr. Nora Volkow sees it differently. “What I like about the new way is that they are putting forward the concept that substance use disorders are dimensional,” she said, meaning that they fall along a continuum.
She compared the condition to obesity. “If you are mildly overweight, we don’t say you have an irreversible disease. You address it so that you don’t progress. I hope that this can facilitate early intervention without necessarily stigmatizing those that are targeted.”
My experience of addiction treatment and reporting on it leaves me less hopeful about this outcome than Volkow. As Frances put it, “Failing to make the distinction at diagnosis will contribute to failing to make the distinction in treatment.” That could leave teens and college students even more prone to being pushed to label themselves—and create issues with future health insurance to boot.
I urge DSM committee members to consider these potential unintended consequences—and avoid them by creating a separate category for a short-term, time-limited substance use disorder that is explicitly defined as not predictive of addiction.
Authors of the earlier edition only belatedly recognized the harm they did to pain patients by conflating “addiction” and “dependence,” and the confusion the physiological vs. psychological dependence issue produced around cocaine. It would be tragic if the DSM V simply shifts from harming one group of patients to overdiagnosing another and unnecessarily promotes an addiction epidemic in the next generation.
Maia Szalavitz is a columnist at The Fix. She is also a health reporter at Time magazine online, and co-author, with Bruce Perry, of Born for Love: Why Empathy Is Essential—and Endangered (Morrow, 2010), and author of Help at Any Cost: How the Troubled-Teen Industry Cons Parents and Hurts Kids (Riverhead, 2006).
